
For me, one of the most infuriating aspects of health care is the relegation of mental health problems, and mental health services, as secondary to physical health.
There are a myriad of examples of this, from the classic stigma that people with mental health problems receive compared to those with physical health problems (fantastically illustrated by the Robot Hugs comic), to the way in which deficiencies in physical care make front page news while mental health services wither in relative obscurity (have you seen any national headlines about staffing problems on mental health wards? Yeah, me neither…).
The lack of physical health treatment for people with serious mental illness is a particularly ugly twist on this. We know for example that people with long-term physical health problems can have their depression ignored or minimised (Coventry et al. 2011), in line with the problems above where mental health is considered secondary or somehow less important.
In people with severe mental illness (SMI), the opposite seems to occur: their physical health needs and problems seem to be ignored because only the management of their mental health problem is considered (see (De Hert, CORRELL, et al. 2011) for a quite devastating review of all the different physical health problems which are more common, or less effectively treated, in patients with SMI).
This is called ‘diagnostic overshadowing’, where negative stereotypes or assumptions about symptoms lead to physical health being less thoroughly treated or recognised (Thornicroft 2011). I almost wish I could say that’s because in this case the mental illness is the priority, but it’s really another example of neglect. In this case, the narrow focus on managing only the mental health problem means ignoring the person who has that problem, and their wider needs. Perhaps worse than the scenario where services ignore the mental health problem, in this case it seems they only manage the mental health problem, and ignore the person instead.
The cost of this to that person has been quantified: people with SMI die on average up to 20 years earlier than the rest of the population, and the cause of death is predominantly untreated physical illnesses. While some of this is attributable to medication side effects and lifestyle factors (not that those can be dismissed – the severe physical costs of some medications and the fact that people with SMI tend to have more vulnerable lifestyles are serious problems in themselves), there are also clear disparities in access to care and health professional screening of problems (De Hert, Cohen, et al. 2011).

Diagnostic overshadowing can lead to physical health problems going unnoticed in people with severe mental health problems
To try to address this, there have been various calls for better screening of problems in patients with SMI and attempts to improve management and monitoring of physical health in this group. One approach is to encourage GPs/family doctors to give more physical advice to patients with SMI, and that’s what this recent Cochrane review aimed to explore (Tosh et al, 2014).
Methods
- The review covered all randomised clinical trials focusing on general physical health advice for people with serious mental illness
- They included 7 studies comprising 1,113 patients in total. Six of these compared provision of advice to standard care. They weren’t able to properly compare different types of advice giving as these analyses were “grossly underpowered”. (You know statisticians are cross when they roll out the word ‘grossly’)
- They evaluated the quality of the included studies
Results
On the whole, results were unimpressive. Two studies indicated that provision of advice led to greater uptake of health prevention services and more contact with primary care, but overall the studies were of low quality and results equivocal. Consequently, with the state of current evidence being as it is, it isn’t possible to determine whether there are benefits of general physical health advice, or actually whether there may be risks of clinicians spending time and effort on something that is ineffective.

Primary researchers run the gauntlet with Cochrane statisticians if they produce low quality trials
Conclusions
Attempts to synthesise the evidence were limited by poor design and poor reporting. The authors note that it was unclear in most studies if randomisation was done properly, and that three of the studies were sponsored by pharmaceutical companies, which raises concerns about the independence of the findings. They were, quite rightly, again A Bit Cross:
Much data were often reported in such a way as to make comparative analyses impossible and we were unable to report data for many outcomes.
I applaud the authors for their plea (on page 30 of the review) for researchers to sign up to the AllTrials campaign to encourage better reporting and greater transparency. The campaign calls for all trials to report all methods and results, so that we can actually make use of the data produced, which is given to us, remember, by patients themselves who have agreed to take part. Those patients deserve better. The patients paying up to 20 years of life deserve better too.
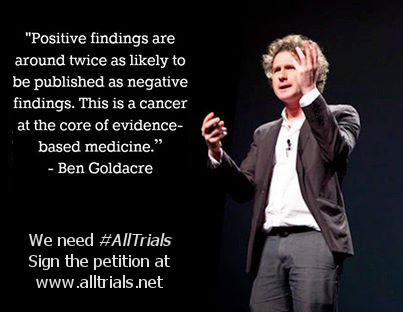
We’ve said it before and we’ll keep saying it until #AllTrials are published. Sign up and support the campaign now!
NB. There’s a very good plain language summary for the review. Possibly the reason it’s so good is that it’s been written by a member of the audience so to speak (Ben Gray from Rethink) rather than by the research team, a practice I would heartily encourage other reviewers to follow.
Links
Tosh G, Clifton AV, Xia J, White MM. General physical health advice for people with serious mental illness. Cochrane Database of Systematic Reviews 2014, Issue 3. Art. No.: CD008567. DOI: 10.1002/14651858.CD008567.pub3.
Coventry, P.A. et al., 2011. Talking about depression: a qualitative study of barriers to managing depression in people with long term conditions in primary care. BMC Family Practice 2011, 12:10 doi:10.1186/1471-2296-12-10
De Hert, M., CORRELL, C.U., et al., 2011. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry, 10(1), pp.52–77.
De Hert, M., Cohen, D., et al., 2011. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World psychiatry: official journal of the World Psychiatric Association (WPA), 10(2), pp.138–151.
Thornicroft, G., 2011. Physical health disparities and mental illness: the scandal of premature mortality. The British Journal of Psychiatry, 199(6), pp.441–442.


RT @Mental_Elf: We don’t know if general health advice improves physical health for patients with serious mental illness http://t.co/BWcKhY…
We don’t know if general health advice improves physical health for patients with serious mental illness http://t.co/3VoOUHZ3eY
We don’t know if general health advice improves physical health for patients with serious mental illness: For … http://t.co/z69CJMERbz
@dr_know bemoans the lack of studies on the benefits of physical health advice for people with severe mental illness http://t.co/BWcKhYD6af
@Mental_Elf @dr_know lack of studies on benefits of physical health advice for people with SMI http://t.co/I1LIHngF4G no parity of esteem!
Why is physical health of people with #mentalhealth problems neglected? http://t.co/i3P6vVZQBY @Dr_Know looks at diagnostic overshadowing.
The Mental Elf liked this on Facebook.
Paula Gardiner liked this on Facebook.
RT @Mental_Elf: Poor screening and lack of access to therapy contribute to poor physical health in severe mental illness http://t.co/AUMQjG…
RT @dr_know: My latest @Mental_Elf blog: 1,113 patients in trials, and still ‘impossible to analyse’. http://t.co/iv9TGMfAHL why we need #a…
RT @Mental_Elf: The scandal of the 20 year mortality gap in severe mental illness: can health advice make a difference? http://t.co/BWcKhYD…
Poor quality studies mean we can’t conclude if health advice approves outcomes for patients w/ severe mental illness http://t.co/AUMQjGJKI5
A question for several elves and a request for multi-disciplinary elving. There are high rates of preventable premature mortality among people with Learning Disabilities and people with SMI. Is this simply because of similar ignorance, stigmatisation and diagnostic overshadowing in healthcare? Could it be that both groups are subsets of a larger group that faces increased risks of illness and is neglected in or discriminated against by health services. How do death rates for unemployed, homeless, low-waged, non-literate, socially isolated compare? What about boring old socio-economic status? Some of these effects are about the specifics of being a person living with mental illness or intellectual disabilities but to what extent does LD or SMI simply stand in as a marker or proxy for poverty? It would be unusual for health service access to be the only, or even the main, determinant of premature death. What are the elves missing when they look at each group of early dead separately?
Hampshire Healthcare Library Service liked this on Facebook.
Vivien Kemp liked this on Facebook.
Gill King liked this on Facebook.
RT @Mental_Elf: Don’t miss: We don’t know if general health advice improves physical health for patients with serious mental illness http:/…
RT @Mental_Elf: 1,113 patients in a review of severe mental illness trials and still no conclusions. Why #alltrials is so important http://…
“We don’t know if general health advice improves physical health for patients with serious mental illness.” http://t.co/OK8nsSWUQ2
We don’t know if general health advice improves physical health for patients
http://t.co/AYvNxy8UHn #mentalhealth #mentalillness #mhuk
Joanne Lloyd reporting how pts with schizophrenia emphasised importance of their physical health needs #hsrn14 see: http://t.co/TOxi08qUXq
It was a decade after a diagnosis of schizophrenia that my Hereditary Heamochromatosis was discovered. I wonder how many more people are out there suffering mental illness with undetected elevated ferritin
Hampshire Healthcare Library Service liked this on Facebook.
Vivien Kemp liked this on Facebook.
Gill King liked this on Facebook.
The Mental Elf liked this on Facebook.
Paula Gardiner liked this on Facebook.
General physical health advice for people with serious mental illness http://t.co/wjnkutfwJV #schizophreniaawarenessweek #plustwenty
[…] We don’t know if general health advice improves physical health for patients with serious mental i… – Mental Elf blog – Dr Sarah Knowles – June 2014 […]