
“I have measured out my life with coffee spoons”
– TS Eliot, the Love Song of J. Alfred Prufrock
Mental healthcare, unlike physical healthcare, lacks objective biomarkers, and relies on self-reported problems interfaced with the training and experience of the assessing clinician. Our electronic records are cluttered with different practitioners’ impressions of individuals and their symptoms and difficulties. While those who use services are often asked to report histories and engage in mental state examinations, these are commonly not tracked in a systematic way and too frequently emphasise clinician-focus issues (think: “are you still hearing voices?”). Contemporary practice has attempted to remedy this through the implementation of Patient Reported Outcome Measures (PROMs), assessments designed to seek a patient’s subjective view of their quality of life. But what exactly to measure?
‘Classical’ psychometric tools, such as the PHQ-9 (Kroenke, Spitzer, & Williams, 2001) for depression and the GAD-7 (Kroenke, Spitzer, & Williams, 2006) for generalised anxiety disorder, are typically predicated around making a diagnosis or establishing a severity level, are ‘condition specific’, and fail to capture both comorbidities and wider social functioning (see: Regier et al., 1990 & Kessler et al., 2005). In essence, the scope of these measures is too narrow. This points to the necessity of a broader based PROM that can be used across services and patient groups. These too exist, however most were typically not structured for use specifically with mental health populations, and their validity in these groups has thus been challenged. They may thus miss important and relevant areas of need in those with mental ill-health. This all begs the question, how do we get to a good PROM?
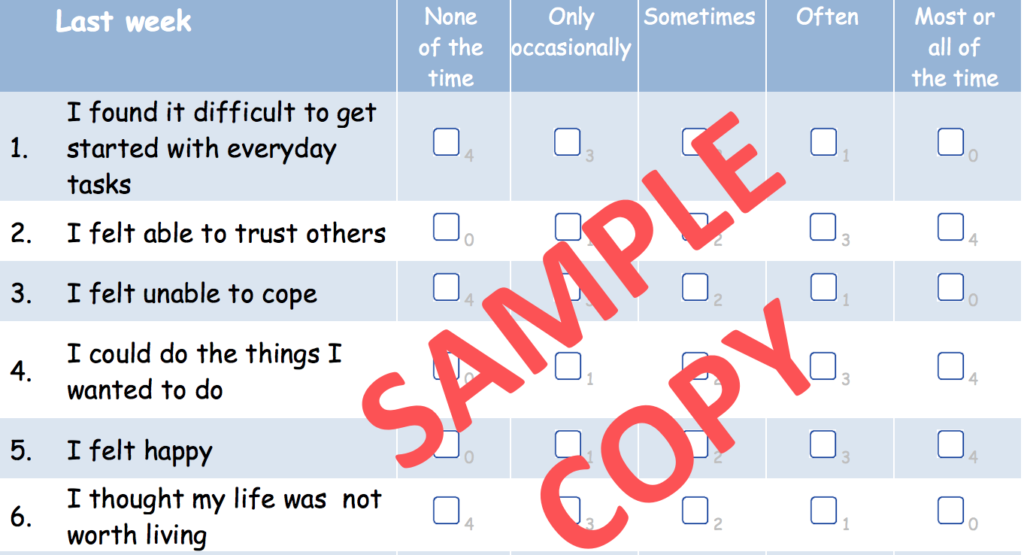
Keetharuth and colleagues attempt to take us there by reconciling the need for more universal measures of quality of life across groups with varying mental health difficulties with the necessity of validity and reliability in clinical tools with the creation of the Recovering Quality of Life (ReQoL) scale (Kaatharuth et al., 2017).

Patient Reported Outcome Measures (PROMs) are assessments designed to seek a patient’s subjective view of their quality of life. But what exactly to measure?
Methods
Keetharuth and colleagues utilised both qualitative methods for item development and initial testing of the scale and quantitative methods to test for validity and reliability.
Prior research was first used to identify themes pertaining to recovery and quality of life: activity, hope, belonging and relationships, self-perception, well-being, autonomy, and physical health. Potential items were generated from interviews and existing PROMs. Item reduction was conducted in multiple phases.
In the first phase, items were winnowed using research literature and consultation with a group of academics, policy makers, clinicians, psychometricians, and service users. Second, 76 service users and 35 clinicians partook in focus groups and interviews and a translatability assessment was utilised to identify future barriers to translations. The third phase consisted of two studies; in study 1, 2,262 participants completed a 61-item set while 4,266 participants completed a reduced 40-item set in the second study. Of these 4,266 participants, 953 completed a follow-up assessment using the same items. Factor analyses were then carried out followed by item response theory analyses. The qualitative data and quantitative data were synthesized then to create a 10-item and a 20-item version of the ReQoL.
2,000 members of the general public and 800 patients were recruited for reliability assessment. Half of the participants completed the 10 item version and the other half the 20 item. A subsample repeated the measures 2 weeks later to analyse test and re-test reliability. Convergent validity was tested by comparing the ReQOL with two other measures (the Short Warwick-Edinburgh Mental Well-being Scale (Tennant et al., 2007) and the Clinical Outcomes in Routine Evaluation (Barkham et al., 2013)).
Lastly, known group validity was evaluated to see whether the ReQoL could discriminate between the general population and those people with specific mental health conditions and responsiveness was measured to look at sensitivity to detection of changes in quality of life.
Results
All response options were endorsed on both the ReQoL-10 and 20 and the full range of scores was covered. Test-retest and internal reliability were both good. The ReQoL correlated highly with existing PROMs suggesting strong convergence among the measures. The ReQoL measures were able to discriminate between patient groups and the non-clinical group. Both versions of the scale detected changes in mental health.

The ReQoL boasts high reliability, validity, and sensitivity.
Conclusions
The ReQoL study included rigorous analyses of its items to find that this new measure is psychometrically sound and considers components of life and recovery that are more important to service users. There is little difference between the 10 and 20 item versions, making both suitable for use.
Strengths and limitations
The greatest strength of the development and testing of the ReQoL is the involvement of service users; over 6,450 were involved as participants and others were involved in the research team. This is important because these are the individuals who have lived experienced of mental health distress and are able to conceptualise what changes are meaningful. Furthermore, the breadth of the questionnaire would allow it to be used across a wide and diverse range of populations.
However, the study does have limitations. The authors acknowledge that randomisation was lacking in their design and all the data were self-reported which is inevitably subject to potential biases and inaccuracy. As is true of almost all PROMs, the issue of subjective value/weight of the various life constructs for individuals cannot be redressed: scoring simply involves summing item response numbers and does not take account of how, for instance, one person may weigh the need to belong much more highly than their activities or autonomy. In fact, it may be the most important aspect of life. If this same person scores a zero on this dimension, they may be considerably unhappy but may still get an overall score that indicates an adequately satisfactory quality of life. However this is the case with all scales: it has been the blog authors’ clinical experience with the CORE-10 that a low total score can lie atop a person high scoring an inability to cope or a sense of despair. The art of practice is using scales to enrich and focus conversations. Keetharuth et al acknowledge this, with the advice that the ReQoL can assist attaining “a more rounded assessment in clinical settings”.

The greatest strength of the development and testing of the ReQoL is the involvement of service users.
Implications for practice
The ReQOL-10 and 20 can be used in routine care and practice as they are short, easy to administer, and score. A license must be requested, however is free for non-commercial and non-commercially funded uses. Support materials such as manuals and translated materials have a fee regardless of use.
Practitioners should take care to look at item responses individually rather than simply looking at the final score. Having a measure that can be used across various care facilities, diagnosis groups, and age groups will allow for easy of transition in care and for comparability across research outcomes. Most importantly, this measure considers what truly matters to patients and will open the pathway to practice revolving around the patient as a person rather than just a cluster of symptoms.
The ReQOL-10 and 20 can be used in routine care, practice, and research.
PROMs have been promoted for some time, but uptake is patchy; some of this is due to a lack of a good, broad measure, which the ReQoL has helped redress; some is due to the challenge of widespread implementation across a larger healthcare organization and system, with ‘real-time’ digital usage and multi-level feedback and analysis for service users, clinicians, teams, and services – a problem as yet generally not cracked. We’ll all be going to the PROM, but it’ll be later than we’d like.
Conflicts of interest
None.
Links
Primary paper
Keetharuth AD, Brazier J, Connell J, et al, on behalf of the ReQoL Scientific Group (2017) Recovering Quality of Life (ReQoL): a new generic self-reported outcome measure for use with people experiencing mental health difficulties. The British Journal of Psychiatry (2017) 0, 1–8. doi: 10.1192/bjp.2017.10
Other references
Kroenke K, Spitzer RL, Williams JB. The PHQ‐9 (PDF). J Gen Intern Med 2001; 16: 606–13.
Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7 (PDF). Arch Intern Med 2006; 166: 1092–7
Darrel A. Regier, Mary E. Farmer, Donald S. Rae, Ben Z. Locke, Samuel J. Keith, Lewis L. Judd, Frederick K. Goodwin. Comorbidity of Mental Disorders With Alcohol and Other Drug Abuse Results From the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511–2518. doi:10.1001/jama.1990.03450190043026 [JAMA Abstract]
Ronald C. Kessler, Wai Tat Chiu, Olga Demler, Ellen E. Walters. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication (PDF). Arch Gen Psychiatry.2005;62(6):617–627. doi:10.1001/archpsyc.62.6.617
Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., … Stewart-Brown, S. (2007). The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation (PDF). Health and Quality of Life Outcomes, 5, 63. http://doi.org/10.1186/1477-7525-5-63
Barkham, Michael & Bewick, Bridgette & Mullin, Tracy & Gilbody, Simon & Connell, Janice & Cahill, Jane & Mellor-Clark, John & Richards, David & Unsworth, Gisela & Evans, Chris. (2013). The CORE-10: A short measure of psychological distress for routine use in the psychological therapies (PDF). Counselling and Psychotherapy Research. 13. 1-13.
Photo credits
- Photo by Katya Austin on Unsplash
- Photo by ål nik on Unsplash
- Photo by Ethan Weil on Unsplash

[…] Recovering Quality of Life (ReQOL) scale: a PROM you don’t want to miss […]