
“You are not a real woman!”
“Whatever you have in your pants must be disgusting!”
“You are confused! Let me give you what you like.”
Andrea keeps reviving those traumatic events. When she was transitioning to Andrea at school, some kids didn’t accept her appearance. At university, a group of men made her life one of the most denigrating and distressing experiences anyone can face. Now, Andrea is trying to get help, but she can’t; she has to wait for years. As a result, Andrea has been struggling with substance misuse.
Andrea is a fictional character that portrays the reality of too many transgender people. Studies consistently highlight that transgender people are at more risk of experiencing childhood trauma, bullying and sexual violence (Stotzer, 2009; Marzetti, 2021; Ashdown & Kyriacou, 2022). For instance, about 50% of transgendered people claim to have been forced to have sex at some point throughout their life (Stotzer, 2009). Isn’t this shocking?
A combination of health and social stressors creates the perfect storm for gender minorities to be at a higher risk of mental health difficulties (Gnan, 2019; Meyer, 2003; Marzetti, 2021). Compared to heterosexual people, mental health issues are 2.67 higher (Williams et al., 2021), and suicidal thoughts and attempts are 3 times more likely in people who identify as LGBTQ+ (Marshal et al., 2011).
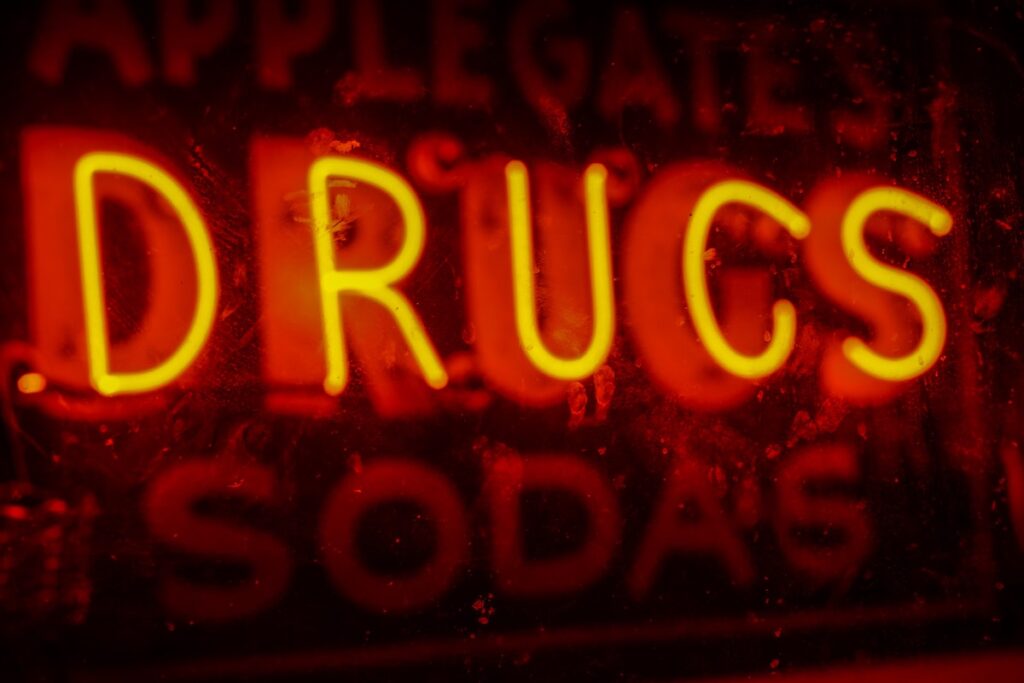
A coping mechanism to deal with mental health difficulties is substance use. The specific social and health stressors suffered by transgender people may put them at higher risk of developing problematic drug use. However, research to develop relevant and effective interventions for transgender people is lacking (Hibbert et al., 2021).
In their recent systematic review, Dean Connolly and Gail Gilchrist (2020) have identified the factors driving substance use in transgender people as well as described the patterns of use within this population. Importantly, they have identified the gaps in the current literature and suggested future directions.
The transgender community often are at higher risk for problematic drug use and healthcare disparities compared to their cisgender counterparts.
Methods
This study was a narrative systematic review that followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. The authors searched for papers in 4 databases: Medline, Embase, PsycINFO and the Global Health database. To filter the literature, they used two types of terms: population (transgender adults, e.g. gender non-conforming) and outcome records (substance use, e.g. chemical sex).
In this study, only primary quantitative studies were included, other academic publications such as qualitative studies and reviews were excluded. Importantly, studies with less than 30 transgender participants were excluded. Both authors independently filtered the records by reading the titles and abstracts. Then, the first author extracted data from these records and the second author-verified 10% of this data. This sample was chosen randomly.
Results
Following the database search, 778 records were identified of which only 41 met the inclusion criteria. More than half of these studies (n=27) were conducted in the US. The remaining studies were from (Canada n=2), Spain (n=2), India (n=2), Brazil (n=2), Cambodia (n=2), Malaysia (n=1), Mexico (n=1), Pakistan (n=1), and the Dominican Republic (n=1).
Together, these studies summed 23,191 transgender participants. They were most commonly recruited through convenience sampling (n = 17) and respondent-driven sampling (n = 9). Overall, the most used sampling techniques (n = 39) were non-probabilistic, and the most common design was cross-sectional (n = 39).
Correlates of substance use
Perhaps the most interesting results yielded by this systematic review were the identified correlates of substance use within the transgender population:
- The studies analysed here consistently found that experiences of transphobic violence were correlated with the use of illicit drugs, alcohol and non-medical prescriptions drugs
- Strikingly, 72% of transgender participants in one study reported drinking alcohol to cope
- Moreover, sex work and gender-affirming hormone therapy were associated with alcohol and illicit drug use in various studies.
Comparing substance use in transgender and cisgender people
The studies that compared alcohol and illicit drug use between transgender and cisgender participants found that the prevalence of substance use is higher and more excessive in transgender people:
- For instance, one study conducted in Canada estimated that heavy episodic drinking is 1.5 times greater in transgender people after controlling for age
- In line with this finding, a handful of studies found that transgender people have a higher risk of developing problematic alcohol use
- Among the studies that compared drug use between transgender and cisgender participants, only 3 considered a range of illicit drugs. These studies found that transgender people were more likely to use illicit drugs compared to their cisgender counterparts
- Specifically, one study found higher rates of cocaine and amphetamine use in transgender people relative to cisgender people.

In this review, transphobic violence, unemployment, sex work and gender dysphoria were associated with a higher prevalence of substance use among the trans community.
Conclusions
The authors identified the following gender-minority correlates of substance use within transgender communities:
- transphobic discrimination or violence,
- unemployment and sex work,
- gender dysphoria,
- gender expression incongruent with societal expectation and
- intersectional sexual minority status.
Together, these factors might explain the higher and more excessive prevalence of drug use in the transgender population compared to cisgender counterparts.
However, more research is needed. Specifically, non-binary people should be considered in future studies. The scientific literature would also benefit from more studies conducted outside the US and from increasing the diversity of study designs.

Numerous factors may explain the problematic drug use by transgender people, but more research is needed across genders and sexual minorities.
Strengths and limitations
The authors of this paper did an excellent job reviewing the existing quantitative literature on substance use among transgender adults. The paper critically synthesises the findings and produces clear conclusions and recommendations that have immediate implications for academics and clinicians.
Moreover, the authors included tables tabulating the characteristics, correlates and data extracted from the papers. These tables help the reader access the details of the selected papers in a clear and concise manner. Both clinicians and academics will benefit from reading these tables when trying to get a handle on the research performed on this topic.
Although the authors state that qualitative studies were excluded from the search, they don’t provide reasons for this decision nor discuss how including this type of research would have impacted the insights drawn from the analysis of the quantitative literature. The authors claim that a meta-analysis of the findings was not possible given the significant heterogeneity among the selected studies. Thus, qualitative data could have been included and it might have filled some of the gaps identified in the quantitative literature. Finally, the authors could have extracted data about the way the selected studies recorded gender. Given that standard procedures for recording gender aren’t universally and systematically applied, the review would have benefited from including a section about gender recording practices.
Finally, the authors identified two limitations within the studied literature:
- Firstly, the rates of stimulant use might be biased. The revised literature disproportionately focuses on urban transgender women at high risk of HIV. This population has shown the highest prevalence of stimulant use. The authors claimed that ‘this narrow focus on particularly vulnerable transgender women biases estimates of substance use and limits the generalisability of these findings’.
- Secondly, the reviewed literature lacks a comparison of substance use behaviours between binary and non-binary transgender people. The literature also lacks studies that only focus on transgender men. All studies included either both populations or transgender women only.

This systematic review provides a clear and critical examination of quantitative studies exploring substance use among transgender adults.
Implications for practice
Andrea shouldn’t have suffered from bullying or sexual abuse. If she had not lived these traumatic experiences, she would have had more chances of not developing a problematic relationship with drugs. Inclusive education should be nurtured at all levels in the journey of any individual (Ashdown & Kyriacou, 2022). However, given the urgency and complexity of the issue at hand, multi-level interventions to improve the quality of life and mental health of transgender people are needed.
The findings in this systematic review have two main implications for clinical practice:
- Gender identity should be recorded to adapt interventions accordingly, given the stigma and trauma faced by many transgender people
- Previous studies have also advocated for increasing gender diversity training among mental health professionals (Strauss et al., 2020).
Lastly, more research is needed to understand the risk factors for problematic drug use among transgender people. Clinicians can immediately contribute to this lack of understanding by implementing the first recommendation.

Clinicians should record gender identity, implement trauma-informed interventions and develop effective treatments targeting trans people.
Understanding alcohol use in UK transgender and non-binary communities
Dr Dean Connolly and Dr Emma Davies from Oxford Brookes University have recently launched a survey to find out more about the positive and negative experiences of alcohol use in the UK transgender and non-binary (trans) population. To date, trans people have been overlooked in UK alcohol use research. This is, in part, because historical measures of gender haven’t considered that gender may exist beyond the binary (male/female) or that it may differ from birth-assigned sex. They hope that by addressing this lack of representation we can begin a dialogue that will inform both future research and the development of relevant health messages and inclusive alcohol reduction services, with the overarching aim of making alcohol use safer for trans people.

Please share this survey across your networks, to help us learn more about alcohol use in trans people.
Statement of interests
From the 1st of February to the 31st of March, the first author of the primary paper and the writer of this blog, in collaboration with others, are promoting a survey about alcohol consumption in UK transgender and non-binary communities. Based on this survey, they will produce academic articles, among other outputs. The writer of the blog will be an author in at least one of the academic publications. Additionally, the writer is the director of Drugs and Me, a social enterprise which aims to make drug use safer. Drugs and Me receives donations through PayPal and Patreon to support our content, software and research work. Drugs and Me is one of the main partners promoting the survey. The writer is also co-founder and shareholder of NeuroSight, a social enterprise that aims to prevent drug-related harm.
Links
Primary paper
Connolly, D., & Gilchrist, G. (2020). Prevalence and correlates of substance use among transgender adults: A systematic review. Addictive Behaviors, 111, 106544. [ScienceDirect abstract]
Other references
Hibbert, M. P., Hillis, A., Brett, C. E., Porcellato, L. A., & Hope, V. D. (2021). A narrative systematic review of sexualised drug use and sexual health outcomes among LGBT people. International Journal of Drug Policy, 93, 103187. [PubMed abstract]
Ashdown, Andie & Kyriacou, Theophanis. Childhood trauma, bullying-victimisation and the mental health of LGBTQ+ individuals (Article). The Mental Elf, 6th Jan 2022.
Stotzer, R. L. (2009). Violence against transgender people: A review of United States data. Aggression and Violent Behavior, 14(3), 170-179. [PubMed abstract]
de Visser, R. O., Wheeler, Z., Abraham, C., & Smith, J. A. (2013). ‘Drinking is our modern way of bonding’: young people’s beliefs about interventions to encourage moderate drinking. Psychology & health, 28(12), 1460-1480. [Taylor&FrancisOnline abstract]
Marzetti, Hazel. Risk factors for LGBTQ+ youth self-harm and suicide (Article). The Mental Elf, 6th Jul 2021.
Strauss, P., Lin, A., Winter, S., Waters, Z., Watson, V., Wright Toussaint, D., & Cook, A. (2021). Options and realities for trans and gender diverse young people receiving care in Australia’s mental health system: findings from Trans Pathways. Australian & New Zealand Journal of Psychiatry, 55(4), 391-399. [SAGE abstract]
(2019) General and LGBTQ-specific factors associated with mental health and suicide risk among LGBTQ students. Journal of Youth Studies. DOI: 10.1080/13676261.2019.1581361
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin, 129(5), 674. [PsycNet abstract]
Marshal, M. P., Dietz, L. J., Friedman, M. S., Stall, R., Smith, H. A., McGinley, J., … & Brent, D. A. (2011). Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. Journal of adolescent health, 49(2), 115-123. [PubMed abstract]
Williams, A. J., Jones, C., Arcelus, J., Townsend, E., Lazaridou, A., & Michail, M. (2021). A systematic review and meta-analysis of victimisation and mental health prevalence among LGBTQ+ young people with experiences of self-harm and suicide. PloS one, 16(1), e0245268. [PubMed abstract]
Photo credits
- Photo by Emily Bernal on Unsplash
- Photo by Jorge Saavedra on Unsplash
- Photo by Danilo Alvesd on Unsplash
- Photo by Lena Balk on Unsplash

Other limitations on studies of substance use (and other health outcomes) among transgender people.
– almost all (if not all) rely on selective sampling therefore making prevalence comparisons are undermined
-furthermore given we have no reliable population prevalence of trans status i am not sure how a reliable prevalence can be calculated.
– prevalence comparisons dont appear to control for age (a major factor in substance use) and it is not clear if they compare prevalence or consumption with the same biological sex eg trans women with males) or with the gender identity (trans women with females) this would have an enormous impact as sex as prevalence rates are far higher among males.
– generally we need better record keeping and data collection on transgender status if we are to properly understand the trans health experience. current data collection is not up to scratch.