
When Lenore C. Terr published her article on “childhood traumas: an outline and overview” 30 years ago (Terr, 1991), she certainly was not the first to recognise that adverse early life experiences could result in myriads of clinical presentation; traumatic childhood experiences were some of the basis of Freud’s psychoanalytic theories, which was further expounded by his daughter Anna Freud (Yorke, 1996).
Although Lenore’s observations were brilliantly classified, provocatively described and theoretically compelling, the level of evidence was some notches below what was required to show a causal association between trauma and mental disturbances. However, features of her described type II trauma (Terr, 1991) bears striking similarity to the current definition of complex trauma – a set of severe experience usually occurring in childhood or adolescence, that involved multiple events of interpersonal assaults or threats (Lewis et al., 2021; UK Trauma Council, 2021)
Sadly, the true prevalence and total impact of childhood traumas will probably never be known as most cases are private and often go unreported. As such, the abuse prevalence of 18.6% in children (UK Trauma Council, 2021) and the reported 1 in 5 adults who experience abuse in the UK is worrying, as it is likely to be an underestimation (Office for National Statistics, 2020).
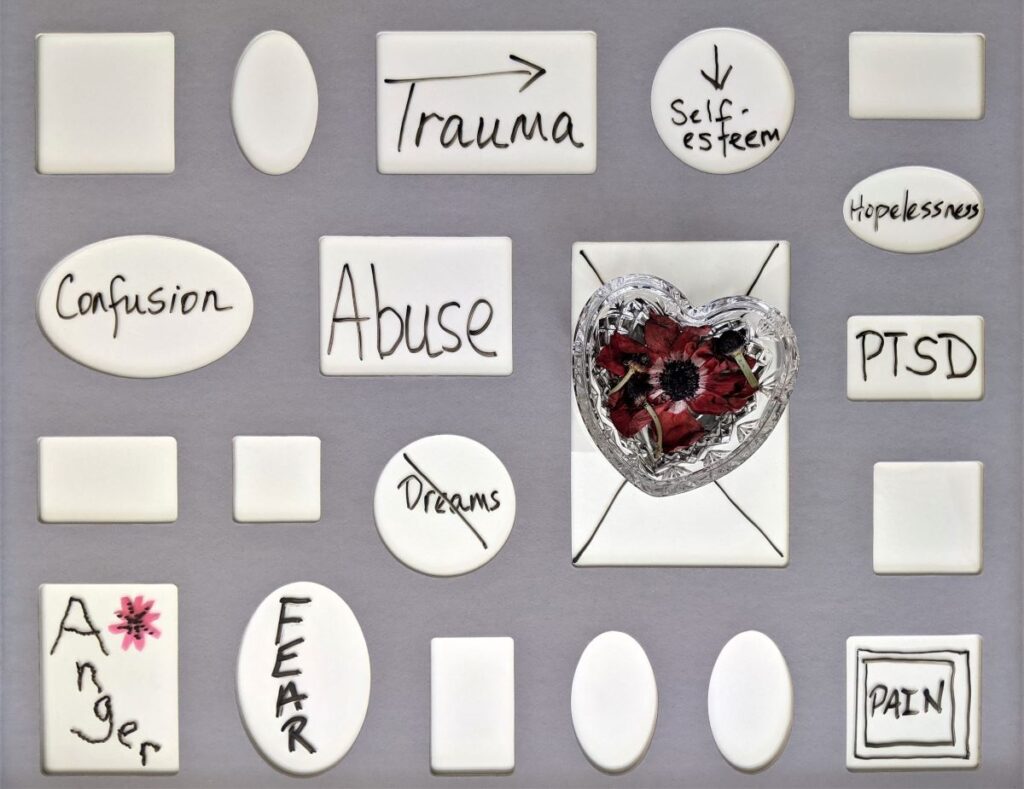
Many quantitative studies have evidenced the association between complex trauma and the development of general and specific mental health disorders (Dube et al., 2001; Webb et al., 2017) beyond the popular and historical link with PTSD (Sara and Lappin, 2017).
To further our understanding of the effect of complex trauma and mental health problems, Stephanie Lewis and colleagues in their recently published work uniquely explored the contribution of pre-existing vulnerabilities to the link.

Sadly, the true prevalence and total impact of childhood traumas will probably never be known as most cases go unreported.
Methods
Participants were recruited from the E-Twin Register and comprised of 2,232 British children born between 1994-1995. Participants were followed up over 13 years from the initiation of the register in 1999-2000 and were assessed at ages 5 (baseline), 7, 10, 12 and 18 (final) years old. Families were recruited to be representative of the UK population and the sample represented the full range of socioeconomic conditions in the UK, as reflected in the families’ distribution on a neighbourhood-level socioeconomic index A Classification of Residential Neighbourhoods. There was no statistically significant difference in the demographics of the study participants from baseline to completion.
Complex trauma was defined using operationalised criteria based on the relevant literature and assessed at interview at the age 18 using the DSM-5 PTSD Criterion A and Juvenile Victimization Questionnaire. Participants were categorised based on their exposure as: complex trauma exposed, non-complex trauma exposed and no trauma groups.
The team combined symptoms from 11 assessment scales for various mental health disorders to derive an aggregate measure of general psychopathology. Participants were also evaluated for nine psychiatric disorders (in the last year):
- ADHD
- Major depressive disorder
- Generalised anxiety disorder
- Conduct disorder
- Alcohol dependence
- PTSD
- Cannabis dependence
- Nicotine dependence
- Psychotic symptoms.
General intelligence was tested at 18 years using an abridged version of the Wechsler Adult Intelligence Scale (Wechsler, 2008), while specific domains of cognitive functions (executive function and processing speed) were assessed with relevant battery.
Preselected early childhood vulnerabilities (internalising/externalising symptoms, IQ at 5 years, proportion of family members with history of mental illness, socioeconomic status and sex) associated with both dependent and independent variables were assessed at baseline.
The role of genetics and/or shared environmental factors was assessed by examining correlation between differences in trauma exposure and the presence of psychopathology or cognitive deficit within twin pairs.
Results
The results followed 3 major themes in line with the aims of the research.
1. Is complex trauma exposure associated with…
a) … More severe psychopathology compared with the trauma unexposed group?
- Both trauma exposed groups scored higher on general psychopathology; the complex trauma group had twice the effect size of the non-complex trauma group.
- Participants exposed to complex trauma had more specific psychiatric disorders on mean count and highest prevalence across all the categories of psychiatric disorder assessed.
- The non-complex trauma group had higher count than the non-trauma exposed group and were more likely to experience five (1-5 above) of the nine listed disorders.
b) … Poorer cognitive deficits compared with the trauma unexposed group?
- Participants with complex trauma had the lowest IQ scores and performed poorest on measures of executive function and processing speed.
- The non-complex trauma group were not significantly different from the trauma unexposed group in their IQ scores and performance on cognitive subdomains.
2. Is greater early childhood vulnerability associated with higher risk of complex trauma exposure?
- All preselected vulnerabilities except IQ at the age of 5 were significantly associated with higher risk of complex trauma exposure over no trauma exposure.
- A similar association was seen with complex trauma over non-complex trauma, except that family history became insignificant. However, family history of mental illness was the only vulnerability significantly associated with non-complex trauma over no trauma.
3. Do early childhood vulnerabilities account for…
a)… Psychopathology linked to complex trauma?
- In all group comparisons, the presence of childhood vulnerabilities did not account for the association of trauma with psychopathology, however the magnitude of effect of the trauma was reduced.
- In genetic analysis, complex trauma was associated with general psychopathology independent of family environment and genetic factors.
b)… Cognitive deficits linked to complex trauma
- Early childhood vulnerabilities accounted for association of trauma exposure with cognitive deficits in the inter-group and intra-group comparisons.
- There was no relationship between complex trauma and IQ score in general when family and genetic influence were controlled for.

Internalising/externalising symptoms, proportion of family members with history of mental illness, socioeconomic status and sex at age 5 were all significantly associated with higher risk of complex trauma exposure over no trauma exposure.
Conclusions
Exposure to trauma had a severity related relationship to the development of psychopathology and the presence of cognitive difficulties. Complex trauma exposed participants had higher psychopathology and lower cognitive scores compared to non-complex trauma or no trauma exposed participants.
While most of the pre-existing vulnerabilities in the study predicted a higher risk of experiencing complex trauma and explained the majority of the cognitive difficulties, they did not account for the association of complex trauma with psychopathology.
Genetic and family environment did not affect the association of psychopathology with exposure to complex trauma but largely accounted for the cognitive difficulties associated with exposure to complex trauma.
Exposure to trauma has a severity related relationship to the development of psychopathology and the presence of cognitive difficulties.
Strengths and limitations
The authors explored an issue of clinical and public health concern and the research was robust in terms of the follow-up and measures of most variables in the study. The analysis was clear and presented in a relatively simple and understandable format. The attrition rate was low as 93% of participants completed the study.
The operationalisation of the complex disorder criteria helps to define the construct and perhaps lays the foundation for future studies on the subject. The author looked beyond PTSD as an outcome which is popular in literature and found significant associations with other categories of mental illness.
Retrospective reports of trauma exposure are subject to recall bias and could misconstrue the strength and association of the findings. In addition, traumatic experiences by nature are prone to distortions and may affect how events are recalled (Strange and Takarangi, 2015). Time of traumatic experience has been also shown to be related to development of psychopathology with proximal reportage likely to have a higher effect on psychopathology (Croft et al., 2019).
Blurring of the temporal interval between exposure and outcome assessment undermines the inference of causality, the article thus entertained a bias that the stated study design usually mitigates against. It is vital that research attempts to strengthen causal inferences through study design and analysis (Danese, 2020) as much as practically feasible.
Although self-report is a popular approach to obtaining reports of trauma, verification of information through records or prospective assessment of caregivers/participants would have strengthened the findings as in other studies (Schaefer et al., 2017; Croft et al., 2019).
No justification was mentioned for the selection of the 11 scales for general psychopathology in the article; mental and behavioural disorders with three of the nine individual categories of diagnosis appears over-represented. Furthermore, the diagnostic categories are highly comorbid conditions; there was no explanation of how this was approached in the paper as individual count of diagnosis would overestimate the association with complex trauma or skew association to reported disorders.
Psychosis was analysed as a separate diagnostic category in the study, no such categorisation currently exists in both ICD-10 and DSM-5 (World Health Organization, 1993; American Psychiatric Association, 2013). It is possible that psychotic disorders (schizophrenia, bipolar and acute psychotic disorders) were too small to report individually or be useful in statistical analysis. This could have been highlighted by the researchers.
The operationalisation of the complex disorder criteria helps to define the construct and perhaps lays the foundation for future studies on the subject.
Implications for practice
Primarily, it is imperative that services identify and support people with existing vulnerabilities as they are more likely to experience complex trauma. In taking history from patients, clinicians need to evaluate vulnerabilities and characterise severity of traumatic experiences to provide commensurate services and support.
Assessment of trauma, whenever present, should be robust and comprehensively focus on all possible impact of trauma; nonetheless, individual causal inference of mental disorder maybe too simplistic and premature. A biopsychosocial formulation of causation with temporal relationship of factors is clinically useful in management of patients.
Complex trauma is multifaceted and is thought to act through a common pathway, further research is needed to fully understand this pathway, the variabilities of component experience, and individual threshold. Research should also be in the direction of understanding protective factors and assessing services.
The literature on general psychopathology makes an interesting read (Caspi et al., 2014; McElroy et al., 2018; Allegrini et al., 2020); it echoes the over two centuries old unitary concepts (INHN: Bulletin 29 : Wilhelm Griesinger and Unitary Psychosis (Einheitpsychose), 2018) and dissatisfaction with current classification system. Classification remains the soft underbelly of psychiatry, the need for more research into the biological basis of diagnostic categories in psychiatry cannot be overemphasised.

Assessment of trauma, whenever present, should be robust and comprehensively focus on all possible impact of trauma; nonetheless, individual causal inference of mental disorder may be too simplistic and premature.
Statement of interests
The author declared no conflicting interest in the article.
Links
Primary paper
Lewis, S., Koenen, K., Ambler, A., Arseneault, L., Caspi, A., Fisher, H., . . . Danese, A. (2021). Unravelling the contribution of complex trauma to psychopathology and cognitive deficits: A cohort study. The British Journal of Psychiatry, 219(2), 448-455. https://doi.org/10.1192/bjp.2021.57
Other references
Allegrini, A. G. et al. (2020) ‘The p factor: genetic analyses support a general dimension of psychopathology in childhood and adolescence’, Journal of Child Psychology and Psychiatry, 61(1), pp. 30–39
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association
Caspi, A. et al. (2014) ‘The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders?’, Clinical Psychological Science : a Journal of the Association for Psychological Science, 2(2), pp. 119–137
Croft, J. et al. (2019) ‘Association of Trauma Type, Age of Exposure, and Frequency in Childhood and Adolescence With Psychotic Experiences in Early Adulthood’, JAMA psychiatry, 76(1), pp. 79–86
Danese, A. (2020) ‘Annual Research Review: Rethinking childhood trauma-new research directions for measurement, study design and analytical strategies’, Journal of Child Psychology and Psychiatry, 61(3), pp. 236–250
Dube, S. R. et al. (2001) ‘Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study’, Journal of the American Medical Association, 286(24), pp. 3089–3096
INHN: Bulletin 29 : Wilhelm Griesinger and Unitary Psychosis (Einheitpsychose) (no date). Available at: https://inhn.org/cn/home/cordoba-unit/education/educational-series/wilhelm-griesinger-and-unitary-psychosis-einheitpsychosebulletin-29.html (Accessed: 8 July 2021)
Lewis, S. J. et al. (2021) ‘Unravelling the contribution of complex trauma to psychopathology and cognitive deficits: a cohort study’, The British Journal of Psychiatry, 219(2), pp. 448–455
McElroy, E. et al. (2018) ‘Developmental stability of general and specific factors of psychopathology from early childhood to adolescence: dynamic mutualism or p-differentiation?’, Journal of Child Psychology and Psychiatry and Allied Disciplines, 59(6), pp. 667–675
Office for National Statistics (2020) Child abuse in England and Wales, Office for National Statistics.
Sara, G. and Lappin, J. (2017) ‘Childhood trauma: psychiatry’s greatest public health challenge?’, The Lancet Public Health. Elsevier Ltd, pp. e300–e301
Schaefer, J. D. et al. (2017) ‘Adolescent Victimization and Early-Adult Psychopathology: Approaching Causal Inference Using a Longitudinal Twin Study to Rule Out Noncausal Explanations’:, https://doi.org/10.1177/2167702617741381, 6(3), pp. 352–371
Strange, D. and Takarangi, M. K. T. (2015) ‘Memory distortion for traumatic events: the role of mental imagery’, Frontiers in Psychiatry, 6(27), pp. 1–4,
Terr, L. C. (1991) ‘Childhood traumas: An outline and overview’, in American Journal of Psychiatry. Am J Psychiatry, pp. 10–20
UK Trauma Council (2021) Complex trauma | UKTC. Available at: https://uktraumacouncil.org/trauma/complex-trauma (Accessed: 7 July 2021)
Webb, R. T. et al. (2017) ‘Self-harm and violent criminality among young people who experienced trauma-related hospital admission during childhood: a Danish national cohort study’, The Lancet Public Health, 2(7), pp. e314–e322
Wechsler, D. (2008) Wechsler Adult Intelligence Scale. Fourth, Archives of Clinical Neuropsychology. Fourth. Pearson.
World Health Organization (1992) ‘The ICD-10 Classification of Mental and Behavioural Disorders’, International Classification, 10, pp. 1–267.
Yorke, C. (1996) ‘Anna Freud’s Contributions to Our Knowledge of Child Development: An Overview’, Psychoanalytic Study of the Child. Yale University Press, pp. 7–24
Photo credits
- Photo by Alex Blăjan on Unsplash
- Photo by Luke Pennystan on Unsplash
- Photo by Nick Fewings on Unsplash
- Photo by Susan Wilkinson on Unsplash
- Photo by Thiago Cardoso on Unsplash
- Photo by Glenn Carstens-Peters on Unsplash

I belong to the generation who has personal trauma, generational trauma and trans generational trauma. One size may not fit all.
It may give you the comfort, support & knowledge needed but it is not a miracle cure/work. A full recovery of trauma depends on how much you invest in you. You may need to explore many ways until you find the right method that works for you.
Isn’t this what life is all about? Ironic!
It is all up to the individual & how your are going to make sense of your experiences, your symptoms, your senses, your body, your surroundings, people in your life, your education, your job and all other.
Understanding your trauma is perhaps about making sense of your layers, giving permission to be free, free to live in peace, free to enjoy the life, free to love the self, free to support each other and many more.