
Most of us (70% of the general population) will go through a traumatic or otherwise stressful experience at some point in our lives (Knipscheer et al., 2020). From losing a loved one to surviving a natural disaster, the nature and circumstances surrounding these events vary from person to person. However, they have an analogous capacity to shape us; overwhelming our ability to cope and function.
Complex trauma typically occurs in childhood or adolescence and is characterised by repeated exposure to threats of an interpersonal nature such as abuse or community violence (“Complex trauma – UKTC”, 2022). Our understanding of complex trauma is still in its infancy, and the lack of conceptual clarity regarding its core features and sequelae fuels debate surrounding the existence of the construct (Van Nieuwenhove & Meganck, 2017).
The links between trauma exposure and outcomes such as reduced cognitive functioning and elevated risk of psychopathology are well established. However, emerging evidence (from a small number of cross-sectional studies) suggests that the consequences of complex trauma are more severe than non-complex forms of trauma. For instance, a study by Greeson (2011) found that exposure to complex trauma increased the odds of having at least one mental health diagnosis by 21.3%.
The study authors sought to address some of the existing knowledge gaps by conducting a longitudinal exploration of the links between complex trauma and psychopathology and cognitive deficits, and considered the role of pre-existing vulnerabilities in the origins of these presentations (Lewis et al, 2021).
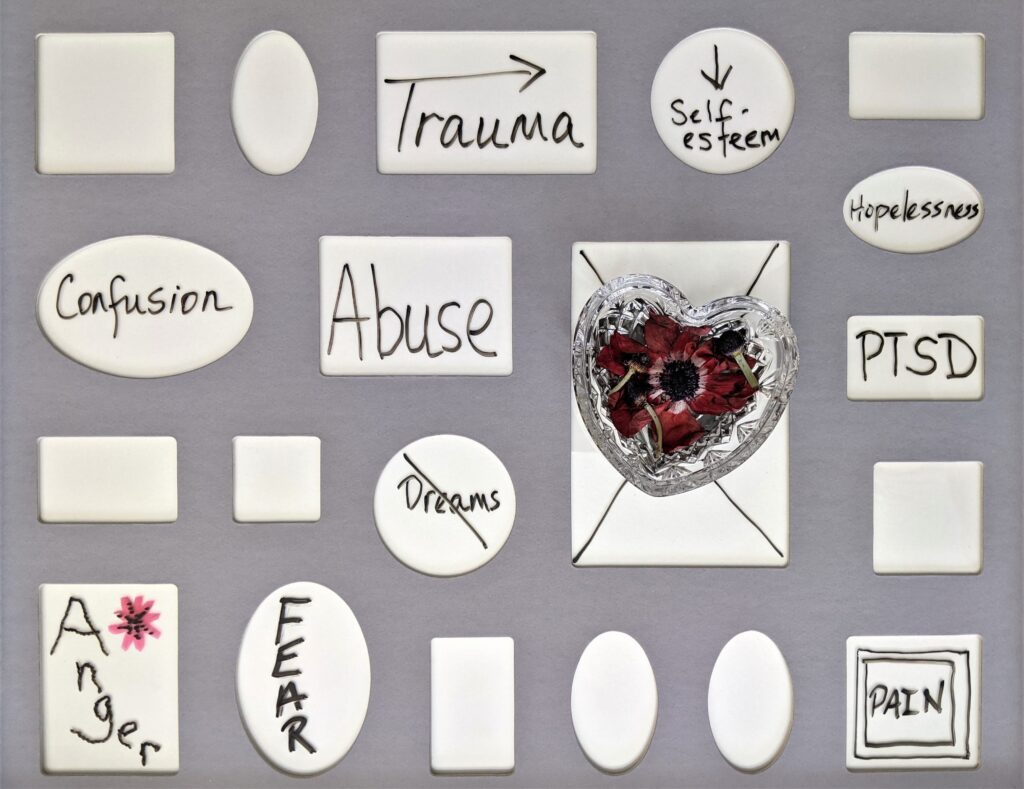
Preliminary evidence suggests complex trauma, characterised by repeated traumatic experiences of an interpersonal nature, is associated with an elevated risk of mental illness compared to non-complex trauma.
Methods
Participants were sampled from the Environmental Risk Longitudinal study. The 2,232 British children included were recruited to be representative of the population, reflecting a range of socioeconomic conditions and evenly distributed across sex. An initial home visit was conducted when children were 5 years old; at which point the authors prospectively assessed for potentially confounding early childhood vulnerabilities known to be associated with trauma exposure, psychopathology and cognitive deficits. These included: internalising and externalising symptoms, IQ, proportion of family members with a history of mental illness, family socioeconomic status and sex.
Subsequent follow-up visits were conducted at 7, 10, 12 and 18 years old. Private interviews were conducted with participants at 18 years old to assess for variables including: lifetime exposure to trauma, past year psychopathology and cognitive functioning.
To compare the relationship between the relevant variables across different subgroups (complex trauma exposed, non-complex trauma exposure, trauma unexposed), generalised estimating equation regression models were fitted (accounting for clustering within families) and group differences tested.
Results
Is complex trauma exposure associated with more severe psychopathology?
Participants exposed to trauma were more vulnerable to severe psychopathology than trauma unexposed participants. Those exposed to complex trauma had higher levels of general psychopathology and were more likely to experience a range of psychiatric diagnoses such as PTSD, depression and psychotic symptoms than those exposed to non-complex trauma.
Is complex trauma exposure associated with poorer cognitive function?
Compared to the trauma unexposed and those exposed to non-complex trauma, participants exposed to complex trauma had lower IQs and poorer functioning on a range of measures of executive functioning and processing speed. However, there was no significant difference between non-complex trauma exposed and trauma unexposed individuals in terms of cognitive function.
Is greater early childhood vulnerability associated with higher risk of complex trauma exposure?
The majority of early childhood vulnerabilities were associated with an increased risk of complex trauma exposure above non-complex and no trauma exposure. However, the only vulnerability associated with a higher risk of non-complex trauma exposure above no trauma exposure was family history of mental illness.
Do early childhood vulnerabilities account for psychopathology linked to complex trauma?
Childhood vulnerabilities did not account for the relationship between trauma exposure and psychopathology. Moreover, within twin pairs (N=1,033) individuals exposed to complex trauma presented with increased psychopathology compared to their twin. This indicates the presence of an association between complex trauma and psychopathology that is independent of genetics or familial environment.
Do childhood vulnerabilities account for cognitive deficits linked to complex trauma?
Early childhood vulnerabilities largely accounted for the relationship between complex trauma and measures of cognitive function such as IQ and executive function. There was no difference in IQ within twin pairs exposed to varying levels of trauma (i.e. complex vs non-complex and trauma unexposed), suggesting that the relationship between these variables is underpinned by familial and genetic factors at the individual level.

Complex trauma-exposed participants experienced higher levels of psychopathology than those exposed to non-complex trauma.
Conclusions
The authors conclude that:
By conflating complex and non-complex traumas, current research and clinical practice underestimate the severity of psychopathology, cognitive deficits and pre-existing vulnerabilities linked with complex trauma

The findings illustrate that the severity of psychopathology, cognitive deficits and pre-existing vulnerabilities linked with complex trauma has been underestimated within research and clinical practice.
Strengths and limitations
Where previous research has typically drawn on clinical and convenience samples, the use of a large representative sample is a key strength of this study. Given the associations between socioeconomic status and vulnerability to trauma exposure, the emphasis on establishing and maintaining an even socioeconomic distribution provides greater confidence in the generalisability of these findings across groups.
However, the sample consists solely of British born individuals, thus findings from divergent birth cohorts could differ. Moreover, the use of a twin design is advantageous for evaluating the potential contribution of genetics and shared environment, but it reflects a lack of randomisation which further limits the generalisability. Although, the study authors do consider this, making reference to comparative findings in singleton-based studies.
The longitudinal approach provides insight into the developmental trajectory of the relevant outcomes; particularly concerning the role of pre-existing vulnerabilities in predicting complex trauma and explaining the association with cognitive deficits. However, our understanding of the emergence of psychopathology and cognitive deficits in relation to trauma remains limited due to the delayed retrospective assessment of outcome variables at a single time point, with responses potentially susceptible to recall and self-report bias.
The authors utilise a broad range of measures of psychopathology and cognitive function, whilst also considering the role of pre-existing vulnerabilities which strengthens our grasp of the qualitative differences between complex and non-complex trauma exposure. However, as noted by the authors “the findings are only valid within the boundaries of their measures”, meaning they fail to account for early traumatic experiences (before the age of 5) which are masked by the adjustment for pre-existing vulnerabilities at 5 years old and unlikely to have been recalled at follow-up.

The use of a broad range of measures of psychopathology and cognitive function in this study provides a deeper grasp of the qualitative differences between complex and non-complex trauma exposure.
Implications for practice
Our understanding of the impacts of complex trauma remains limited, however, the findings suggest that previous conflation of complex and non-complex trauma has resulted in a gross underestimation of the severity of negative mental health outcomes specific to experiencing complex trauma.
It is clear that greater attention to detail is necessary when considering the broad mental health needs of people exposed to complex trauma; thus emphasising the need for a comprehensive approach to assessment in both research and clinical practice. This could encompass a broader evaluation of the nature and severity of trauma experienced, as well as an enhanced exploration of the potential impacts on psychological and cognitive functioning.
In line with current guidance, the study findings support the value of taking a preventative approach to tackling the impact of complex trauma on wellbeing. By being proactive in assessing individuals for vulnerability factors, services could facilitate early identification and support for those most vulnerable to experiencing complex trauma. Beyond this, steps can also be taken to mitigate the potential impacts of complex trauma exposure, for instance adopting a trauma-informed approach within clinical practice and treating mental health problems based on individualised formulation of needs. This blog (Zarska, 2022) provides a useful outline of some of the key principles of effective trauma informed services as reported by service users and carers.
Despite the novel insights provided, the study gives rise to several further questions. Namely:
- What is the mechanism underlying the association between complex trauma exposure and psychopathology?
- What is it about complex trauma that results in more severe psychopathology and poorer cognitive functioning (i.e. qualitative or quantitative difference?).
Further investigation of these questions could inform the development of new, more effective interventions for mental illness in people exposed to complex trauma.
Finally, as professionals, we must exercise caution and avoid making oversimplistic and reductive causal inferences about the relationship between mental health difficulties and complex trauma exposure. Critique of the ACEs (adverse childhood experiences) framework has stressed how taking a deterministic view of trauma exposure can lead to both the perpetuation of stigma and an increase in preventable statutory interventions (Welsh Government, 2021). Thus, it is crucial not to lose sight of the individual when considering the contribution of complex trauma to mental health problems.

By proactively assessing for vulnerability factors, services could provide timely preventative support to those most vulnerable to experiencing complex trauma.
Statement of interests
None.
Links
Primary paper
Lewis, S., Koenen, K., Ambler, A., Arseneault, L., Caspi, A., & Fisher, H. et al. (2021). Unravelling the contribution of complex trauma to psychopathology and cognitive deficits: a cohort study. The British Journal Of Psychiatry, 219(2), 448-455. doi: 10.1192/bjp.2021.57
Other references
Complex trauma – UKTC. (2022). Retrieved 27 May 2022, from https://uktraumacouncil.org/trauma/complex-trauma
Greeson, J. K. P., Briggs, E. C., Kisiel, C., Layne, C. M., Ake, G. S., III., Ko, S. J., Gerrity, E. T., Steinberg, A. M., Howard, M. L., Pynoos, R. S., & Fairbank, J. A. (2011). Complex trauma and mental health in children and adolescents placed in foster care: Findings from the National Child Traumatic Stress Network. Child Welfare, 90(6), 91–108.
Knipscheer, J., Sleijpen, M., Frank, L., de Graaf, R., Kleber, R., ten Have, M., & Dückers, M. (2020). Prevalence of Potentially Traumatic Events, Other Life Events and Subsequent Reactions Indicative for Posttraumatic Stress Disorder in the Netherlands: A General Population Study Based on the Trauma Screening Questionnaire. International Journal Of Environmental Research And Public Health, 17(5), 1725. doi: 10.3390/ijerph17051725
UK Trauma Council. (2022). Complex trauma: evidence-based principles for the reform of children’s social care [PDF]. London. Retrieved from https://uktraumacouncil.link/documents/UKTC-ComplexTrauma-Principles.pdf
Van Nieuwenhove, K., & Meganck, R. (2017). Interpersonal Features in Complex Trauma Etiology, Consequences, and Treatment: A Literature Review. Journal Of Aggression, Maltreatment &Amp; Trauma, 28(8), 903-928. doi: 10.1080/10926771.2017.1405316
Welsh Government. (2021). Review of Adverse Childhood Experiences (ACE) policy: report. Cardiff: Welsh Government.
Zarska, A. (2022). Trauma-informed care in mental health: why we need it and what it should look like [Blog]. Retrieved from https://www.nationalelfservice.net/mental-health/ptsd/trauma-informed-mental-health-care/
Photo credits
- Photo by Thought Catalog on Unsplash
- Photo by Susan Wilkinson on Unsplash
- Photo by Ilya Chunin on Unsplash
- Photo by Usman Yousaf on Unsplash
- Photo by William Warby on Unsplash
- Photo by Malvestida on Unsplash
