The paper reviews the evidence for increased microglial activity in schizophrenia, such as post-mortem evidence and smaller studies including negative studies.
Microglial cells, or microglia, are the resident macrophages of the Central Nervous System. Macrophages are immune system white cells that “eat” foreign material such as bacteria and other material such as cancer cells, as well as interact with the rest of the immune system, amongst many other functions. They get called different names depending on where they are found in the body (e.g. Kupfer cells in the liver). They are also a lot more active and mobile than previously thought, as well as possibly having a role in pruning neuronal synapses (the junctions between nerve cells) (Hughes, 2012).
Methods
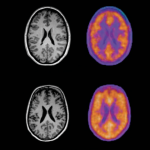
It’s a very complicated method used by the authors. I can’t tell a voxel from a Vauxhall so struggled to follow the more technical aspects. Essentially they used a 2nd generation radio ligand [11C] PBR28 which specifically binds to 18kD translocator-protein (TSPO), which is found on microglia. This is a radioactive molecule which binds to TSPO and thus “labels” a microglial cell.
When the subject has a PET scan after being injected with [11C] PBR28, a brighter signal is detected in areas with more microglia. To identify where these areas are, an MRI brain scan is also performed separately for each subject to generate an accurate picture of that individual’s brain. The PET signal is overlaid on the MRI scan so that areas of brightness can be correlated with areas of the brain.
Amongst the problems the authors faced was that genetics strongly affected how strongly [11C] PBR28 radio ligand bound to TPSO so the genetically mediated “affinity” status (high, low or mixed) was measured. Other problems included the high ratio of “noise” to “signal” that is the final end-result, was to a degree, unreliable.
Two separate cohorts were measured:
- 14 Ultra High Risk of Psychosis cases v 14 Controls
- 14 Schizophrenia cases v Controls
Each case was matched for age with a control. The two cohorts were analysed separately.
All participants were given a Beck’s Depression Inventory (BDI). Ultra High Risk of Psychosis participants were assessed with the Comprehensive Assessment of the At Risk Mental State (CAARMS). Participants with a diagnosis of schizophrenia were assessed with the Positive and Negative Syndrome Scale (PANNS).
Reasonable exclusion criteria were applied such as no recent anti-inflammatory medication or no recent benzodiazepines. Two of the Ultra High Risk of Psychosis cases had exposure to Citalopram antidepressant and the schizophrenia patients were on antipsychotics.
Adjustments were made for age (as it affected microglial activity) and for affinity status and medication status (in Ultra High Risk of Psychosis cases). Particular interest was paid to the frontal and temporal lobe regions, but 2 areas of the brain were used as “control regions” (brain stem and cerebellum).

Can you tell a voxel from a Vauxhall?
Results
For Ultra High Risk of Psychosis (UHRP) cases v controls
- Total grey matter UHRP had higher microglial activity (Cohen’s D= 1.244, i.e. a large effect size) p=0.004
- Frontal grey matter UHRP had higher microglial activity (Cohen’s D =0.894, i.e. a large effect size p=0.03). This effect persisted taking into account Citalopram exposure
- Temporal lobe grey matter UHRP had higher microglial activity (Cohen’s D= 0.829, i.e. a large effect size) p=0.047, but significance of effect lost after taking into account Citalopram exposure
- No significant differences in control regions
For schizophrenia (SCZ) cases v controls
- Total grey matter SCZ had higher microglial activity (Cohen’s D= 1.769, i.e. a large effect size) p<0.001
- Frontal grey matter SCZ had higher microglial activity (Cohen’s D= 1.245, i.e. a large effect size) p=0.005
- Temporal grey matter SCZ had higher microglial activity (Cohen’s D= 1.430, i.e. a large effect size) p=0.001
- No significant differences in control regions, but brain stem came close at p=0.088
No correlation was found between BDI scores and microglial activity or between PANNS scores and microglia in participants with schizophrenia.
There was a significant correlation between CAARMS score and microglial activity (r=0.730, p=0.01).

These findings suggest that neuroinflammation is linked to the risk of psychosis and related disorders.
Strengths and limitations
- Small study
- Took into account individual affinity for the radio ligand
- Ultra High Risk of Psychosis group were antipsychotic free and mostly had limited exposure to psychotropic medications
- Unable to control for antipsychotic exposure in participants with schizophrenia, though the paper suggests this is likely to reduce microglial activity, i.e. reduce the difference between control participants and participants with schizophrenia
- Problem with high “noise” to “signal” ratio means less confidence with results, but large effect sizes showing increased microglial activity mitigates this uncertainty
- CAARMS score showed correlation with increased microglial activity, but PANNS didn’t, meaning uncertain relationship between psychotic symptoms and microglial activity
- Possible progressive relationship of increased microglial activity in Ultra High Risk of Psychosis, then further increased still in schizophrenia
- No 95% confidence intervals for effect sizes to help judge likely range of “true” value
What does this all mean?
It’s a preliminary study that indicates there may be increased microglial activity in people with Ultra High Risk of Psychosis or schizophrenia. Larger studies including unmedicated first episode of schizophrenia participants should be performed.
If the finding does prove to be true what are the implications?
It would need to be established if this happens just in psychosis (or types of psychosis) or happens generally in mental health problems. We would also like to find out the relationship between microglial activity and the psychosis. Is it a cause of psychosis or a reaction to a cause?
If we intervene to reduce (or increase) microglial activity, what effect does it have on the outcomes for psychosis, i.e. is it a good target for an intervention? It should be noted that if increased microglial activity is a reaction to a process causing psychosis, this does not mean the cause is necessarily biological. We may yet find out that psychosocial causes affect the brain to increase inflammation including microglial activity. However, this does add to a large body of evidence that brain processes are affected in people with schizophrenia.

Is microglial activity a cause of psychosis or a reaction to a cause?
Links
Primary paper
Bloomfield PS, Selvaraj S, Veronese M, Rizzo G, Bertoldo A, Owen DR, Bloomfield MAP, Bonoldi I, Kalk N, Turkheimer F, McGuire P, de Paola V, Howes OD. (2015) Microglial Activity in People at Ultra High Risk of Psychosis and in Schizophrenia: An [11C]PBR28 PET Brain Imaging Study. American Journal of Psychiatry 2015 http://dx.doi.org/10.1176/appi.ajp.2015.14101358
Other references
Hughes V. (2012) Microglia The Constant Gardeners. Nature Volume: 485,Pages: 570–572 Date published: (31 May 2012) DOI: doi:10.1038/485570a

Microglial activity in psychosis and schizophrenia https://t.co/tlgfq3cP49 #MentalHealth https://t.co/UakaUfSrOj
RT iVivekMisra Microglial activity in psychosis and schizophrenia https://t.co/MZdKpieFGd #MentalHealth https://t.co/YaxHeyXWKB
Microglial activity in psychosis and schizophrenia https://t.co/fQHF4TdHyJ
Today @SameiHuda on increased microglial activity in schizophrenia and high risk of psychosis https://t.co/V5m1OEWpoB
Can’t tell a voxel from a Vauxhall my latest @MentalElf blog https://t.co/jMmIHUHjmr
Hi @Pete_Bloomfield @SameiHuda Is microglial activity a cause of psychosis or a reaction to a cause? https://t.co/V5m1OEWpoB
@Mental_Elf @SameiHuda hi! Well this is the big question at the moment. So far it’s all correlation so we don’t know about the causation 1/2
@Mental_Elf @SameiHuda longitudinal studies and intervention treatment will help to work it out 2/2
@Mental_Elf thanks for sharing The Mental Elf, have a great Friday :) (insight by https://t.co/2IgPgwZUN0)
Can you tell a voxel from a Vauxhall? @SameiHuda can’t, but we still let him blog for us https://t.co/V5m1OEWpoB
@Mental_Elf @SameiHuda Perhaps the title of the blog should have been “Voxel and I”.
@TheLancetPsych @Mental_Elf @SameiHuda joking aside it’s a key issue for the jobbing shrink making sense of research with fMRI
@TheLancetPsych @Mental_Elf @SameiHuda respect to you for having a go Samei and nice appraisal to boot
@TheLancetPsych @Mental_Elf @SameiHuda the morale of the story is choose your voxels wisely & a mutually beneficial relationship will ensue
@mental_elf And right you were since @sameihuda is a very gifted communicator making complicate matters easy and interesting to read !
Inflammation & psychosis ?Easy to read but rigorous information abt a neat small study https://t.co/7qmbSVNr0q by @SameiHuda at @Mental_Elf
Read @SameiHuda on a brain imaging study comparing relative levels of microglial activity https://t.co/V5m1OEWpoB #psychosis #schizophrenia
[…] 1Microglial activity in psychosis and schizophrenia […]
New study by @Pete_Bloomfield et al suggests neuroinflammation is linked to risk of psychosis & related disorders https://t.co/V5m1OEWpoB
Don’t miss: Microglial activity in psychosis and schizophrenia https://t.co/V5m1OEWpoB
Interesting study on ARMS https://t.co/JiWHDzgxzt
Interesting review, it would be good to compare responders to non responders with diagnosis of schizophrenia and also to find out what additional function do the macrophages have in people with schizophrenia.