
Therapy can be a bloody tough slog, especially when you notice annoying things about yourself. Trying to talk about these bits of who we are can often be really difficult to articulate, especially if they’re a bit obscure. Therapy can highlight how fractured and odd the mind can be at times, how we might not have the whole picture of who we are, and how easy it is to give yourself a really hard time. It can be like a family Christmas dinner in your head, but without the nice food and mulled wine.
For most of the time the mind is seemingly neat and together. Look a little closer though and you’ll notice that actually we’re made up of a jumble of processes happening all at the same time; it’s a beautiful feat of orchestration. Look closer still and you might spot the different characters that occupy your thoughts, maybe a parent or a friend pops into your head just before you’re about to post that article online.
Now imagine these characters weren’t just confined to our sense of self, but sounded like they were right next to you, behind you, or surrounding you, seemingly talking as if the person was right there in the room out of your control; and what’s more, some of them are saying cruel things to you.
For those with psychosis, this can be a daily reality. Hearing voices involves a huge range of sensations; sometimes they’re obvious, other times they can be a ‘silent voice’ (Humpston et al, 2016). Not all voice hearers want to get rid of their voices; just the ones that aren’t exactly helpful or constructive. It makes perfect sense really.
NOTE: Not all those with psychosis hear voices and not all voice hearers have psychosis (Waters et al, 2017). This blog will focus on a study including those with psychosis and who hear voices; these voices tend to be far more negative and distressing (Andrew et al, 2008) than those who don’t need clinical care.
Work in the field (Chadwick et al, 2004) has suggested that trying to conceptualise the voices and characters with an experienced therapist can help take the edge off them; to accept their presence, understand and conceptualise them, and thereby gain some ownership. However, a recent meta-analysis has found effect sizes are consistently small with current techniques.
Now, new digital approaches open up the possibility that those with distressing voices can visually personify their characters and try to create dialogue with them. Will this help improve the efficacy of therapy?
Tom Craig, Phillipa Garrety, and colleagues from the University of Manchester, University College London, and King’s College London investigated how effective a virtual reality (VR) treatment called AVATAR therapy is for distressing auditory hallucinations, compared to traditional supportive counselling (Craig et al, 2017).
Who are you? We might create or relate to our internal characters through computer games, theatre, and art.
Methods
150 participants were equally assigned to either AVATAR therapy or supportive counselling (over 6 weeks), and outcome measures for psychotic symptoms, depression, anxiety, and auditory hallucinations were taken at 12 and 24 weeks.
Participants were either assigned to:
- AVATAR therapy with a skilled clinician in weekly 50-minute sessions over 6 weeks, or
- Supportive counselling sessions with a supervised, graduate psychology assistant.
The details of the supporting counselling sessions are a little hidden in this article, but the authors did mention that they followed the guidelines in a previous research study (Lewis et al, 2002). This details that supportive counselling was conducted over a 5-week period with a total of 15-20 hours per person, including booster sessions at 2 weeks, 1, 2, and 3 months. It’s not entirely clear from the Lancet Psychiatry article (Craig et al, 2017) whether this was followed exactly for this present trial, or whether it was adapted to match the time of individuals in AVATAR therapy. Sessions included themes of quality of life, identity, and coming to terms with previous trauma.
The study was a single blind, randomised control trial at the South London and Maudsley Hospital (only the assessors of therapeutic outcome were blinded to allocation).
Outcomes were measured using a number of valid psychometric questionnaires measuring overall psychotic symptoms, as well as specific qualities of voices, e.g. from the Psychological Rating Scale Auditory Hallucinations subscale (PSYRATS-AH), such as voice frequency, duration, and distress.
Authors calculated, based on results from a previous pilot favouring AVATAR therapy, that 71 participants in each group would be enough for detecting an effect size of 0.6, with enough room for 20% dropout at follow up.
Results
AVATAR therapy was significantly more effective than counselling in reducing scores of distress, negative beliefs, and omnipotence of voices at 12 weeks, but this difference went away at 24 weeks.
- 75 participants were assigned to each group at the start
- At 12 weeks (the primary endpoint), 63 participants remained in the AVATAR group and 61 participants remained in the counselling group
- At 24 weeks, 57 participants remained in the AVATAR group and 58 participants remained in the counselling group
- At 12 weeks, AVATAR therapy was significantly different from counselling in its effect, namely for frequency, distress, and appraisal of omnipotence of voices
- At 24 weeks, AVATAR therapy and supportive counselling ceased to differ in their effectiveness across all measures
- However, between baseline and 24 weeks, both AVATAR therapy and supportive counselling were effective in maintaining reduction of scores on distress in auditory hallucinations
- In fact, those in the counselling group continued to improve between 12-24 weeks, whereas the AVATAR group plateaued.
Conclusion
AVATAR therapy had a significant impact on outcome scores above that of counselling at 12 weeks. However, they look to be equally effective as each other for reducing the frequency, distress, and omnipotence associated with auditory hallucinations in psychosis at 24 weeks.
Perhaps the important questions to ask now are:
- Is AVATAR therapy cost effective and personally useful for patients?
- How can we extend the effects of AVATAR therapy?
Some examples of the avatars created in the study by participants. Therapists assume the role of the avatar during therapy.
Strengths and limitations
I really like this study, I have to say. It uses a new tangible approach to try and create an external, interactive character; something which otherwise might evade language. It captures dynamic and evolving features of voices which the therapist and service user can address as a team.
The sample used is large, participants included were persistently experiencing voices, an active control is used, and the range of psychometrics and co-variables such as cannabis and alcohol use provide neat converging evidence for the effectiveness of AVATAR therapy. This was a well-run first trial.
Saying this, there are a few nagging limitations that I keep coming back to:
- The 24-week follow up scores were not significant between both groups. This is acknowledged by the authors and in the press release, but fairly near the end and not expressed in the abstract. This hypes up the perception of the study to appear much more effective and it’s a little misleading.
- At 24 weeks, supportive counselling wasn’t significantly different from AVATAR therapy. The authors mention that many more topics were covered in counselling sessions than the experimental group, and so it’s a little tough to parse out exactly how the content of sessions made a difference to alleviating symptoms and distress. Including a treatment-as-usual group might be useful for future development. The authors do acknowledge that resource constraints meant this couldn’t be done on this occasion.
- I’m not quite sure what difference is made by using an experienced, skilled therapist in the AVATAR group vs counselling; how can we be sure the specific use of the technology is the key factor here? Could it be replaced with something like art therapy and have the same effect? Having a therapist that is better able to engage with participants might make all the difference, especially if the added value of a skilled therapist encourages participants to be more articulate with their voices.
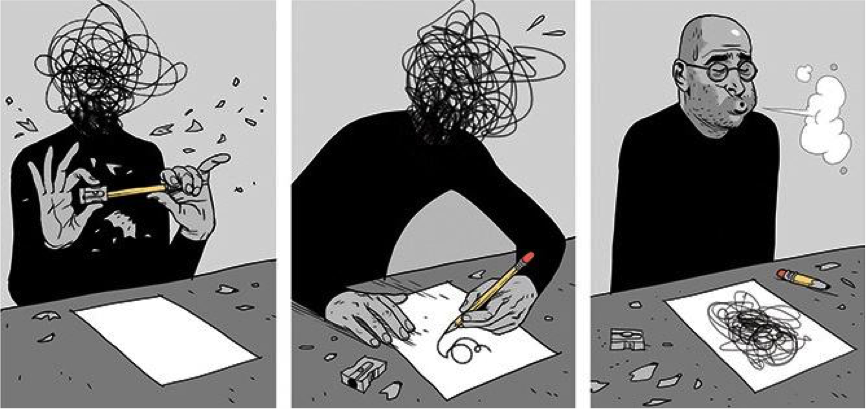
Is the technology providing anything unique? Could this intervention be done just as effectively with art therapy?
Implications for practice
Humans are innately complex, and so are their voices. Individual differences play a huge role in psychological therapies for auditory hallucinations; from nuances in clients to the skill of therapists.
While the AVATAR study shows real innovation and significant clinical effect, there is still a long way to go to pick apart the specific nuances of what works, what doesn’t, and the added value of using the AVATAR method itself.
Conflicts of interest
None to declare
Links
Primary paper
Craig TKJ, Rus-Calafell M, Ward T, Leff JP, Huckvale M, Howarth E, Emsley R, Garety PA. (2017) AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial The Lancet Psychiatry, Available online 23 November 2017.
Other references
Alderson-Day B, Jones N. (2018) Understanding AVATAR therapy: who, or what, is changing? The Lancet Psychiatry, 5(1), 2-3.
Andrew EM, Gray NS, Snowden RJ. (2008) The relationship between trauma and beliefs about hearing voices: a study of psychiatric and non-psychiatric voice hearers (PDF). Psychological medicine, 38(10), 1409-1417.
Bell V. A community of one: social cognition and auditory verbal hallucinations. PLoS Biol 2013; 11: e1001723.
Chadwick P, Birchwood M. (2004) The omnipotence of voices. A cognitive approach to auditory hallucinations. The British Journal of Psychiatry Feb 1994, 164 (2) 190-201; DOI: 10.1192/bjp.164.2.190
Humpston CS, Broome MR. (2016) The Spectra of Soundless Voices and Audible Thoughts: Towards an Integrative Model of Auditory Verbal Hallucinations and Thought Insertion. Rev.Phil.Psych. (2016) 7: 611.
Lewis S, Tarrier N, Haddock G, Bentall R, Kinderman P, Kingdon D, Siddle R, Drake R, Everitt J, Leadley K, Benn A, Grazebrook K, Haley C, Akhtar S, Davies L, Palmer S, Faragher B, Dunn G. (2002) Randomised controlled trial of cognitive-behavioural therapy in early schizophrenia: acute-phase outcomes. The British Journal of Psychiatry Sep 2002, 181 (43) s91-s97; DOI: 10.1192/bjp.181.43.s91
Nayani T, David A. The auditory hallucination: a phenomenological survey. Psychol Med 1996; 26: 177–89.
Thomas N, Hayward M, Peters E. et al (2014) Psychological therapies for auditory hallucinations (voices): current status and key directions for future research. Schizophrenia Bulletin, 40(Suppl_4), S202-S212.
Trower P, Birchwood M, Meaden A, Byrne S, Nelson A, Ross K. (2004) Cognitive therapy for command hallucinations: Randomised controlled trial. Br J Psychiatry 2004; 184: 312–20.
Waters F, Blom JD, Jardri R, Hugdahl K, Sommer IEC. (2017) Auditory hallucinations, not necessarily a hallmark of psychotic disorder. Psychological Medicine, 1-8.
Woods A, Jones N, Alderson-Day B, Callard F, Fernyhough C. (2015) Experiences of hearing voices: analysis of a novel phenomenological survey. Lancet Psychiatry 2015; 2: 323–31.
Photo and video credits
- Plan your FallOut4 character
- AVATAR therapy video from Kings College London press release, 11 Nov 2017
- Sankalpa Art Journeys

I have just looked at this again. This particular approach seems to take the approach of suppressing the voices which seems contrary to the Kings College YouTube ‘Compassion for Voices’. Interesting results in relation to the reduction of distress at three months.