
I came across an unusual paper recently entitled ‘misattributing speech and jumping to conclusions: A longitudinal study in people at high risk of psychosis’ (Winton-Brown et al, 2015). I thought ‘I misattribute speech and jump to conclusions all the time!’ On a more serious note, I am working on a project looking at interventions to help with the self-management of early onset psychosis, so I thought there might be some helpful insights.
Cognitive models of psychosis propose that psychotic symptoms can be the result of poor processing of vague or unclear stimuli (Garety et al, 2007). In particular a key contributing factor is the tendency to use less information to form a decision or jumping to conclusions (Garety et al, 1991).
From my own experience I remember a patient of mine who had schizophrenia. He was a very bright, polite, thin young man in his 20s, always dressed in mismatched colourful clothes. He tended to wear a few more layers than the weather required. He would sit on the edge of the chair giving the impression of a bird ready to take flight. I would normally see him once a week in the ward review. I would have informal chats with him in corridors or out on the street when he was on leave. One day I wanted to discuss some blood test results with him and I invited him to see me in my office. His face paled and he looked extremely worried. ‘You are going to cancel my leave!’ he blurted out. I tried to calm him down and reassure him, but he bolted out of the office before I got the chance. Down the corridor I heard one of the nurses talking him down. Five minutes later he was trying to jump the garden fence convinced that he would never be able to leave hospital. I remember being very surprised as to how that misunderstanding developed so rapidly and had such a great influence on his behaviour. Are those cognitive deficits then something that fundamentally defines the illness?
Research shows that, at presentation, people with at risk mental states have both a tendency to jump to conclusions and problems with verbal self-monitoring. Verbal self-monitoring is determined by presented distorted speech to the individual and asking her or him to make judgements as to whether the speech came from them or from others. People with at risk mental states tend to think their own distorted speech comes from other people rather than themselves (Broome et al, 2007).

People with at risk mental states have both a tendency to jump to conclusions and problems with verbal self-monitoring.
Hypothesis
In this case, the researchers wanted to test that the severity of psychotic symptoms will be chronologically linked to the severity of the cognitive biases. They also tested if the severity of the cognitive biases would predict severity of symptoms and function at follow up.
Methods
The researchers recruited participants with an at risk mental state (as measured with a specific validated instrument) from a London outreach team. They excluded neurological disorders and substance misuse. They assessed them at baseline and on average 31 months later (standard deviation 19). At baseline a range of measures were taken including the positive and negative symptom scale (PANSS), a delusions rating scale and scales rating depression and anxiety, as they felt all those could be factors for developing psychosis. They then used computerised paradigms to measure the severity of the biases towards jumping to conclusions and errors in verbal self-monitoring.
At follow up the two outcomes recorded were the global assessment of function and transition to psychosis using the PACE criteria (Yung, 1998).
Results
Out of the 25 participants recruited at baseline 23 had follow-up data. Forty-eight percent were male, mean age was 24.8 (SD 4.9) and mean IQ 100.2 (SD 10.7).
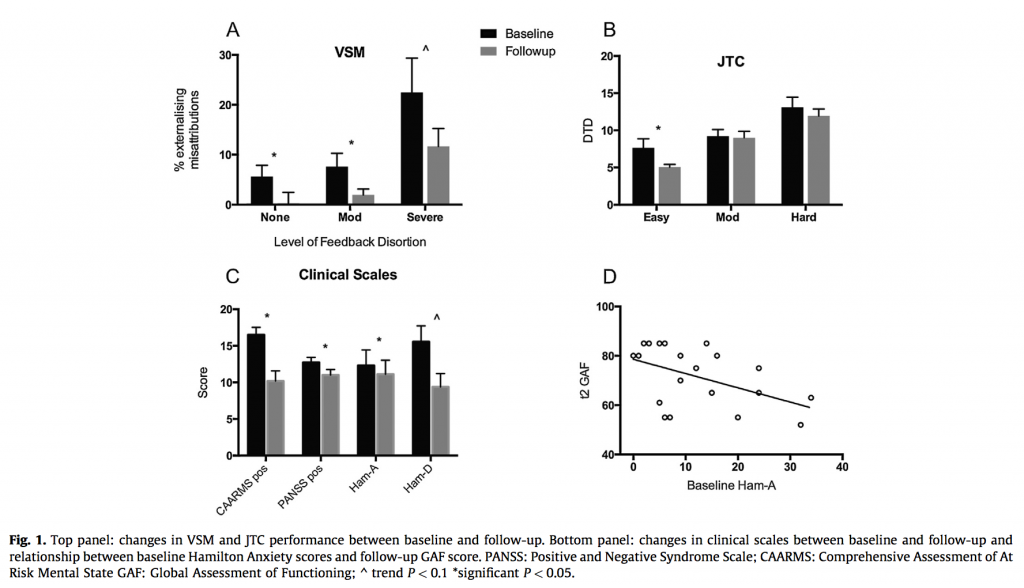
Participants were in treatment during the follow up period and on average their psychotic symptoms improved as did their function. There was a trend towards improvement in their mood symptoms as well.
Verbal self-monitoring improved at follow up but jumping to conclusions remained stable.
Five participants transitioned to psychosis and there was no correlation between progression to psychosis and any of the baseline measures.
The only predictor of function at baseline was the Hamilton Anxiety scale.
Verbal self-monitoring did not correlate to any of the outcomes, but jumping to conclusions correlated with the delusion and hallucination subscores of the PANSS, but not the PANSS score as a whole.
Discussion
There was no correlation between the performance on the cognitive tasks and function or transition to psychosis, but performance on the jumping to conclusions task was correlated with hallucination and delusion scores at follow up. The authors do point out that the number of individuals who transitioned to psychosis was very small making it impossible to draw conclusions. Anxiety was the only predictor of function, a symptom that in psychosis can get ignored in favour of the more salient positive symptoms.
The authors’ conclusion was that psychotic symptoms are related to a jumping to conclusions bias, but this does not predict transition to psychosis or functional outcome.

In this study, only 5 people transitioned to psychosis, so it is impossible to draw any conclusions from this data.
Limitations
- Small sample size leading to underpowered analyses
- The sample population was receiving treatment (psychological and with medication) making it hard to draw conclusions about the natural history of psychosis and the effect of these cognitive biases
- Great variability of duration of follow up so the time of observation could fluctuate significantly from individual to individual, something that is bound to have an effect in such a small sample size
- Excluding individuals with drug misuse makes it hard to apply any learning to the populations most of us are likely to encounter in clinical practice
- The authors performed a large number of statistical analyses with no correction (i.e. they did not perform a multiple test correction, such as a Bonferroni correction)
Conclusion
For me this was a fairly disappointing paper. I understand that it is very hard to find a sample of individuals with at risk mental states that one can reliably follow up for a sufficiently long time, but greater efforts could have been made to find other researchers with similar services to increase that sample size. I do not think I can use anything in this paper to help me decide if I should be worried or not about my patient who immediately thought I was cancelling his leave.
I think I may have learned to pay a lot more attention to symptoms of anxiety in people at risk of psychosis, even though the experiment the authors described was not designed to answer that particular question. Perhaps a better line of research would be exactly that, should we pay a lot more attention to anxiety in psychosis and if we do treat it robustly will we achieve better functional outcomes at follow up?
Any takers?

Should we be paying more attention to anxiety in people with psychosis?
Links
Winton-Brown TT, Broome MR, Allen P, Valli I, Howes O, Garety PA, Johns LC, McGuire P. (2015) Misattributing speech and jumping to conclusions: A longitudinal study in people at high risk of psychosis. Eur Psychiatry. 2015 Jan;30(1):32-7. [PubMed abstract]
Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. (2007) Implications for neurobiological research of cognitive models of psychosis: a theoretical paper (PDF). Psychol Med 2007;37(10):1377–91.
Garety PA, Hemsley DR, Wessley S. (1991) Reasoning in deluded schizophrenic and paranoid patients. Biases in performance on a probabilistic inference task. J Nerv Ment Disord 1991;179(4):194–201. [PubMed abstract]
Broome MR, Johns LC, Valli I, Woolley JB, Tabraham P, Brett C, et al. (2007) Delusion formation and reasoning biases in those at clinical high risk for psychosis (PDF). Br J Psychiatry 2007;51:s38–42. [PubMed abstract]
Yung AR, Phillips LJ, McGorry PD, Jackson HJ, Francey S, McFarlane CA, et al. (1998) Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br J Psychiatry 1998;172(33):14–20. [PubMed abstract]


Are we jumping to conclusions in our understanding of psychosis?: Andrés Fonseca appraises a longitudinal stud… http://t.co/2EyK08vNoX
RT @Mental_Elf: Are we jumping to conclusions in our understanding of psychosis? http://t.co/XBvCDEYjW4
Hi Andres,
I noticed you are working on interventions to help with self-management in early onset psychosis. Do you have anywhere I can find out more information about this? Your work may be of particular interest for a paper I am writing.
Thanks,
Alex
Hi @AndrFon There’s a question from @Mynameisalexio on your blog http://t.co/lZkhmqXiSO
Rosemary Callahan liked this on Facebook.
The Mental Elf liked this on Facebook.
Today @AndrFon looks at misattributing speech & jumping to conclusions in people at high risk of psychosis http://t.co/XBvCDEGJ4w
Olivia Cialdi liked this on Facebook.
Christina Armstrong-Graham liked this on Facebook.
Dr @AndrFon’s article for @Mental_Elf “Are we jumping to conclusions in our understanding of psychosis?” http://t.co/uqprqOZV3M
Hi
looking at a few papers on the subject of jumping to
I suspect
Jumping to conclusions is a marker
Of a cognitive deficit rather than a cause of delusions
Per se
And as we know psychosis can be associated with cognitive deficits
Should we be paying more attention to anxiety in people with psychosis? asks @AndrFon http://t.co/XBvCDEGJ4w
Mental Elf: Are we jumping to conclusions in our understanding of psychosis? http://t.co/vlGOUzmlHV
Are we jumping to conclusions in our understanding of psychosis? http://t.co/t9iomPB62Z via @sharethis
Don’t miss: Are we jumping to conclusions in our understanding of psychosis? http://t.co/XBvCDEGJ4w
@Mental_Elf Great article maybe we shouldn’t necessarily look at symptoms but consider behaviours let’s be open to a non medical conclusion
Impact of anxiety on psychosis – “@Mental_Elf: Are we jumping to conclusions in our understanding of psychosis? http://t.co/2zy1HR7oKS”
One of the biggest diagnostic mistakes is overdiagnosing schizophrenia based on soft signs
http://t.co/8wXgEJU6ld @Mental_Elf
@AllenFrancesMD @Mental_Elf Or based on “availability” of atypical antipsychotics, which makes it “cool” to dx schizophrenia
@AllenFrancesMD @Mental_Elf Maybe an even bigger, actually historic mistake is “diagnosing” schizophrenia at all! We should offer real help.
Most popular blog this week? It’s @AndrFon Are we jumping to conclusions in our understanding of #psychosis? http://t.co/XBvCDEGJ4w
Are we jumping to conclusions in our understanding is psychosis? http://t.co/7KFQQ2R7YE
“@AllenFrancesMD: 1 of biggest diagnostic mistakes is overdiagnosing schizophrenia based on soft signs
http://t.co/oFETTsYOdt @Mental_Elf”
“Jumping to conclusions in our understanding of psychosis?” Via @Mental_elf http://t.co/CzIA8S65ic
“Are we jumping to conclusions in our understanding of psychosis?” http://t.co/r56fO88rr8
My first psychosis was two years ago when I was 80 . It was brought about ,I think, by a combination of anxiety, stress, shock and severe pain.
Dr Andres Fonseca’s article for @Mental_Elf “Are we jumping to conclusions in our understanding of psychosis?” http://t.co/uqprqOZV3M
Never mind jumping to conclusions about anxiety being a marker for Psychosis as a link–especially whilst in a bin–a bin itself is the most anxiety causing environment i know– why are you jumping to conclusions about your patient–why do you people always jump to conclusions– i mean the blokes in the bin isn’t he– Ive never met anyone in the bin who isn’t worried their never going to get out– what are you imagining?your forcefully locking them upo and drugging them– what part about anxious dont you get– in fact the bin threatens their victims with it/(keeping them in their)and say they wont be letting them out until they start talking like they know they have a mental illness and will take the drugs, and the tag, so they have to play the game — aquiesce– or pretend they will do what they want, act how they want them to act in order to get out– its as though you didnt even see the fear you and your people very clearly place on your captives– and if you cant even see that it makes me wonder why you should be able to even be there– wheres the understanding the empathy the common sense even–also if everyone in there is worried about getting out– why dont you realise someone may have said something in a conversation with your poor patient about not getting out seeing as thats what they all fear– and may have even said it again to your patient /victim on his way to your office– get real.
Anyway Who’s to say that even focusing on a bad future– for someone,– let alone prophesying/or predicting it,–for someone– isn’t a bad thing, regardless of what we imagine is wrong-will be wrong, or hope to find– to start with.
maybe its better we all start with intentionally looking for/at goodness together- to help them and us all collectively -winning– as opposed to losing ourself in the thinking of whats wrong— is winning finding out whats wrong with you? i dont know if it is– its what gets people into trouble in the first place– low self esteem– we all know why—- sins and guilt, name calling, nastiness, drugs , alcohol, bullies etc— we effect each other collectively.actions-what we do–visually–how we look, and verbally–what we say feel and think- just be careful about the crystal ball of misery ;-).