
All those debating personality disorder agree it remains a contentious issue in mental healthcare, with suboptimal treatment delivery. Matters are not helped by disagreement on how these diagnoses should be approached. The two major psychiatric diagnostic systems ICD-11 and DSM 5 remain far apart. Governments have invented other classifications to suit overtly political purposes, e.g., Dangerous & Severe Personality Disorder (1). The press reports stories about both the harm such people do (2), and the dreadful things that happen (or don’t) when they seek treatment (3). The paper we (David Foreman and Keir Harding) are blogging about allows us to ask a crucial question: does making the diagnosis do more harm than good?
Though methodologically a review, we are approaching the paper as a case study, with Borderline Personality Disorder (henceforth BPD) being the case in point. It’s a good choice because it is the most identified personality disorder in mental health services (4) and its treatment sufficiently effective to have NICE guidelines (5), which recommend what to do when identified.
We can reframe the question the authors posed as follows: does the harm of receiving a diagnosis with known stigma outweigh the benefits of being potentially signposted to effective treatments? We will first consider:
- What is a “scoping review”?
- Have the authors done enough, methodologically, to answer the question they posed?
Then we will explore whether their answers can help with our ongoing debates and disagreements about BPD and personality disorder more generally.
Does the harm of receiving a diagnosis with known stigma outweigh the benefits of being potentially signposted to effective treatments?
Methods
What is a scoping review?
Scoping reviews are used when it is unclear whether there is sufficient literature to form a well-evidenced, reasoned analysis of the topic of interest (1). This paper mapped the boundaries of our knowledge on stigma in BPD. The authors supplemented searches of relevant academic databases searching with a trawl for “grey literature”. They used thematic analysis, and included a reflexive approach, i.e., attempted to use the authors’ frames of reference as additional interpretative instruments (2). They tried to map both the literature beyond the “walled garden” of peer-reviewed scholarship, and explicitly reflect their own personal biases.
Did the methodology deliver?
Reporting guidelines
Systematic reviews can show rigor by following published reporting guidelines, which constrain investigators to adhere to methodologically sound procedures, and publishing the research design on a repository so changes are clear. Appropriate reporting guidelines were followed, and the protocol was registered, but was subsequently withdrawn pending a resubmission that has not yet occurred. This creates uncertainty about whether the a priori process was followed, i.e. did they actually conduct the review in the way that they originally said they would?
Search strategy
The paper describes considerable care in the development and testing of their exhaustive search strategy. The number of unique publications identified was 3,566; much higher than previously found (3). The inclusion of grey literature, while making sense (as stigma seems more likely to be described there) is a methodological challenge, given its likely lower scholarly quality. The inclusion of reflexivity would contribute to the sensitive inclusion and use of such data.
Quality assessment
The nostrum “garbage in equals garbage out” applies to all reviews, so quality assessment of included articles is vital. The team’s rejection rate of around 10% of their initially included papers on quality grounds (as measured by the Mixed Methods Appraisal Tool – MMAT) seems lower than reports on purely quantitative data (e.g., 4). It is possible that MMAT quality assessments of qualitative literature are less sensitive than their quantitative counterparts. Once again, this is something that reflexivity can address.
Analytic approach
A narrative synthesis is standard for scoping reviews, so any issues will be around implementation. No grey literature made it into the final set of 57 articles. It seems unlikely any relevant scholarly articles were missed. The disappearance of grey literature may be compensated for by the number of included articles which included testimonies. The multi-staged complexity of reflexive narrative analysis has been reduced to a single paragraph, leaving details of the process unclear. However, the authors describe a triangulation process between investigators and service users, which implicitly introduces reflexivity and checks both content (whether coverage has been sufficient) and construct (whether the interpretation is consistent with testimony and experience) validity.

The authors tried to map both the literature beyond the “walled garden” of peer-reviewed scholarship by including grey literature, and explicitly reflect on their own personal biases.
Results
The authors reference “structural stigma” (5) which moves the concept of stigma beyond that of an injury done by prejudiced individuals to a structural characteristic of societal institutions. There is conceptual overlap between this and the Social Construction Theory (SCT) of policy design (6), where groups are mapped on the two dimensions of high versus low political resources and positive versus negative social constructions. SCT predicts that groups which are low/negative in both will find policies are developed to shift societal goods away from them to better positioned rivals. In the context of health service delivery, structural stigma would be applied to politically weak groups which had negative social constructions, and BPD fits such criteria.
Unsurprisingly, they found ample evidence of harmful structural stigma, which they summarise in the chart reproduced below.
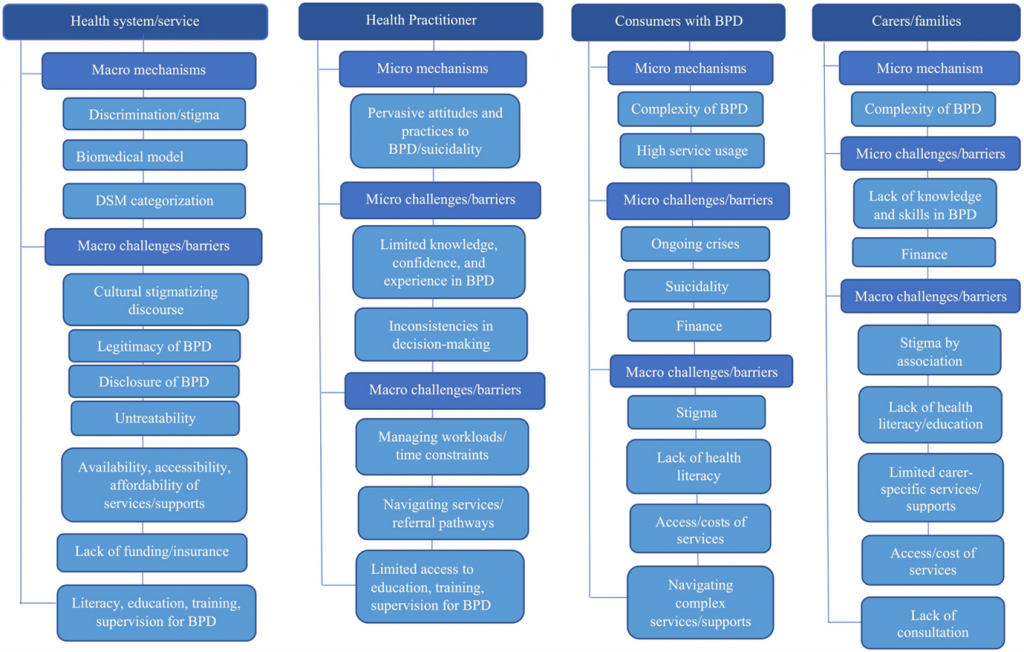
Figure 1: Summary of sources of stigma affecting people with BPD. [View full-sized figure]
David Foreman’s discussion
The authors have attempted a methodologically sound account of all available literature to demonstrate the importance of structural discrimination as a negative influence on the lives of people with BPD. The quality of the evidence and the paper’s methodology provides at least moderate evidence for this overall. I provide my own appreciation using their preferred MMAT tool below.
| Methodological quality criteria | Responses | |||
| Yes | No | Can’t tell | Comments | |
| 1.1. Is the qualitative approach appropriate to answer the research question? | This is standard for a scoping review. | Even though implicit, the use of reflexivity, expressed through triangulated evaluations, is a strength. | ||
| 1.2. Are the qualitative data collection methods adequate to address the research question? | Standards were met. | The inclusion of quality screening was a strength. | ||
| 1.3. Are the findings adequately derived from the data? | Analytic steps were not clear. | The absence of an updated protocol & compressed methods report added uncertainty. | ||
| 1.4. Is the interpretation of results sufficiently substantiated by data? | The biomedical model was not defined & uncritically rejected. | There is no agreed definition of the biomedical model. Examples of incorrect assumptions about biomedical data were assumed to be due to the model without considering practitioner bias for other reasons. | ||
| 1.5. Is there coherence between qualitative data sources, collection, analysis, and interpretation? | There was incoherence around diagnosis, treatment, and the biomedical model. | Diagnosis is central to any biomedical or related model. Service users reported receiving a diagnosis as being of value if they were not simultaneously stigmatised; they also wished to receive treatment. Avoidance of diagnoses was associated with structural stigma and led to exclusion from healthcare. | ||
The authors reported that failure to diagnose led to more exclusion, not access to healthcare by a better route. Rather than debating diagnostic validity, I would point out that these findings are consistent with the predictions of SCT. We should focus instead on the unfair claim that people with BPD have low social value as determining the lack of training investment and false beliefs, despite staff, as well as service users, wanting to do better. People with BPD make valuable contributions to the arts, sciences and literature, and their loss through suicide is a loss to us all, which can be reversed with proper treatment and understanding. The Pride movement, which asserted alternative sexualities and their value, has been successful. The same could happen for BPD, and people with it should not be denied access to the diagnosis: such identification can be, like alternative sexualities, the first step towards political resources.

Klein et al. (2022) reported that a failure to diagnose borderline personality disorder led to greater exclusion from care, rather than access to healthcare by a different route.
Keir Harding’s discussion
Let the quibbling begin! Any Mental Elf reader who follows my blogs will be blown away that I am contributing to a blog that interrogates the value of what is being said in the paper rather than just commenting. Hats off to David for doing that so well. This blog is a great example of confirmation bias as we have both taken different things away from it. Who is right? Possibly both of us, probably neither of us. You decide. The important thing is that two elves can differ in views but still make magic together.
Let me start by saying that this paper is adamant that BPD is a valid diagnosis. There isn’t a hint that a diagnosis where 80% of people have lived through trauma might be a response to circumstances. Where it doesn’t talk about illness, it talks about disease. The authors have not declared their lived experience (if any exists), and I wonder if the acceptance of the validity of the diagnosis would have been as emphatic if that voice had contributed.
The authors tell us that the stigma experienced by people diagnosed with BPD is real. It details experiences that are abusive and discriminatory. These generally occur during interactions with people employed to help.
The authors break the stigma into 5 key themes:
1. Legitimacy of the diagnosis
Clinicians view people with a BPD diagnosis through a moral rather than clinical lens and do not correctly see it as a valid illness/disease.
2. Reluctance to disclose a diagnosis
Clinicians think “this person has BPD” but either don’t tell them or diagnose something else instead. The authors quote a tiny study saying people are glad to be given a diagnosis and are happy if it is given in a thoughtful and compassionate way. There is no evidence about what happens when people walk out of the thoughtful, compassionate clinician’s room into the stigma described in the rest of the article. There is no exploration of how people feel after being told their difficulties make sense, given their experiences and offered appropriate help. It’s as if there are only these two options.
3. Discourse of untreatability
The idea that nothing can help. This is a nonsense of course. There are some chilling staff attitudes around refusing to help people with the diagnosis (it would be unthinkable to say the same things about survivors of abuse).
4. BPD and healthcare
People with the diagnosis will use crisis services more than others and have a rotten experience of it.
5. Practitioner/Consumer interactions
If practitioners are nice things tend to be okay, but often they aren’t.
The authors make the obvious assertion that we need to do better than this. They highlight the inadequacy of the medical model (which has a substantial influence on the article). They emphasise that some practitioners lie to their patients about their diagnosis because telling them would “do more harm than good”. This paper is emphatic about the cost of being given the label. The key message for me here is “DO NOT LIE TO YOUR PATIENTS!”. Tell people they meet the criteria for something. Tell them it could be added to their notes. Remember you have no control over how people treat them once they are out of your clinic.
What baffles me is that the paper contains reams of negatives regarding the BPD diagnosis, but the idea of ditching it isn’t mentioned. Perhaps we should respond to people on the basis that they have survived hell, rather than on the basis that there is something intrinsically wrong with them. In the twenty years since No Longer A Diagnosis of Exclusion (2003) highlighted the poor treatment people receive in the UK, the stigma has not changed. Do we give it another 20 years? Another 40? I suggest we see the last 20 years as a failed experiment in challenging stigma and start again.
In the UK, perhaps we are starting again. The Royal College of Psychiatrists has assembled a panel of clinicians and people with lived experience to look at stigma, labels, and alternatives to the current diagnosis. I am grateful to the authors for detailing the horror this diagnosis can bring, but I am amazed that more radical responses to the stigma were not considered.
*As an example of confirmation bias at work you’ll notice I ignored everything I agreed with.

Keir Harding states, “Perhaps we should respond to people on the basis that they have survived hell, rather than on the basis that there is something intrinsically wrong with them… I suggest we see the last 20 years as a failed experiment in challenging stigma and start again.”
Statement of interests
David Foreman is a Child and Adolescent Psychiatrist. He is affiliated (in various ways) to the Royal College of Psychiatrists, the National Institute for Health and Care Excellence, the Institute for Psychiatry Psychology and Neuroscience at King’s College London, and the Centre for Values-Based Practice, St Catherine’s College, Oxford. He diagnoses personality disorders in his clinical practice, and previously blogged his views at https://psychobabel.blog/2017/08/06/personality-and-its-disorders/
Keir is an Occupational Therapist and clinical lead for Beam Consultancy. He is on the executive committee of the British and Irish Group for the Study of Personality Disorder and is a member of the Royal College of Psychiatrists Expert Reference Group for Stigma, Labelling and Personality Disorder. He helps people diagnosed with ‘personality disorder understand themselves differently and blogs his views here.
Links
Primary paper
Klein, P., Fairweather, A.K. & Lawn, S. Structural stigma and its impact on healthcare for borderline personality disorder: a scoping review. Int J Ment Health Syst 16, 48 (2022). https://doi.org/10.1186/s13033-022-00558-3
Other references
1. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018 Nov 19;18(1):143.
2. Campbell K, Orr E, Durepos P, Nguyen L, Li L, Whitmore C, et al. Reflexive Thematic Analysis for Applied Qualitative Health Research. Qual Rep [Internet]. 2021 Jun 20 [cited 2023 May 4]; Available from: https://nsuworks.nova.edu/tqr/vol26/iss6/24/
3. Ring D, Lawn S. Stigma perpetuation at the interface of mental health care: a review to compare patient and clinician perspectives of stigma and borderline personality disorder. J Ment Health. 2019 Mar 12;1–21.
4. Webster R, Liu R, Karimullina K, Hall I, Amlôt R, Rubin G. A systematic review of infectious illness Presenteeism: prevalence, reasons and risk factors. BMC Public Health. 2019 Jun 21;19.
5. Hatzenbuehler ML. Structural stigma: Research evidence and implications for psychological science. Am Psychol. 2016 Nov;71(8):742–51.
6. Schneider A, Sidney M. What Is Next for Policy Design and Social Construction Theory? Policy Stud J. 2009;37(1):103–19.
Photo credits
- Photo by Pablo García Saldaña on Unsplash
- Photo by Kelly Sikkema on Unsplash
- Photo by Annie Spratt on Unsplash
- Photo by Markus Spiske on Unsplash
- Photo by Markus Spiske on Unsplash
