
Can we encourage patients to continue taking complementary and alternative (CAM) treatments for antenatal depression or should we be firmly discouraging them from doing so?
We already know from surveys that 11% of primary care patients with anxiety and depression are taking complementary or alternative therapies, which is around the same proportion of people who take an antidepressant for depression. So pregnant woman are likely already using CAM treatments – do they help?
Antenatal depression is common: more than one in ten women will experience it during their pregnancy. It presents a complex treatment decision – untreated or inadequately treated depression has consequences for both the mother and the developing fetus, and no currently used treatment comes without its drawbacks.

There are numerous herbal remedies freely available to pregnant women
Antidepressants have proven efficacy in depression but knowledge about their safety comes only from observational studies which cannot rule out long terms risks of fetal exposure. Psychological therapies are also effective, but can take twelve weeks or more to work, may not be appropriate in severe depression and patients may not have universal access to these treatments.
Complementary and alternative therapies have therefore drawn considerable interest by researchers interested in avoiding these drawbacks as well as amongst patients who subscribe to the mantra ‘natural is better’.
There are a plethora of treatments that are considered complementary or alternative:
- Physical therapies – bright light therapy, physical exercise, yoga, acupuncture, sleep deprivation
- Nutraceuticals – omega-3 fatty acids, tryptophan, SAM-e, folic acid, inositol, amino acids, alpha-lactabumin, DHEA and acetyl-L-carnitine
- Herbal remedies – St John’s Wort, Crocus sativus, Lavandula angustifolia, Rhodiola rosea and Gingko biloba as wellas a variety of other leaves, flowers, roots, bark and berries
Methods
The Cochrane Pregnancy and Childbirth Group undertook a review of studies exploring CAM treatments. They included published and unpublished randomised controlled trials of ‘acceptable quality’.

You know you’re getting old when systematic reviewers start to look young
They found 18 trials examining these treatments of which they deemed only 6 to be high enough quality to report. The 12 studies were excluded for a variety of reasons – including lack of randomisation, lack of blinding of the assessor to group allocation, lack of a control group and because the women examined were either healthy women or experiencing postpartum, rather than antenatal depression.
The authors reported that the methodological quality of the studies included was still not strong – the sample sizes were below 100, except for two of the trials and for most of the interventions only one suitable study was included.
- In the studies included depressive symptomatology was measured using either the HSRD or BDI;
- treatment response meant a greater than 50% reduction in HSRD scores;
- and remission indicated a final HSRD score of less than 8.
Studies reported either a mean difference (MD) between groups in the case of continuous variable, or a risk ration (RR) in the case of a categorical variable.
Results
Four CAM treatments were evaluated:
Remedial maternal massage
-

Pregnant women – listen up! This review shows that massage from your partner during pregnancy may help to reduce symptoms of antenatal depression
Two trials, with 38 and 88 participants, compared maternal massage with non-specific acupuncture and found no significant differences between the two groups in rates of clinical depression, depressive symptomatology or treatment response
- A third trial (148 participants) compared maternal massage provided by the woman’s partner to standard care and found a significant decrease in depressive symptomatology (MD= -6.7, 95% CI -9.77 to -3.63)
Acupuncture
- In 35 women assigned to either depression-specific acupuncture (according to traditional Chinese medicine principles) or non-specific acupuncture there was no difference detected in rates of clinical depression or depressive symptomatology immediately following treatment, but treatment response was greater in those given the depression-specific acupuncture (RR 1.68, 95% CI 1.06 to 2.66)
Bright light therapy
- Bright light therapy was compared to a dim light control (27 participants) and a significant reduction in depressive symptomatology was found (MD -4.80, 95% CI -8.39 to -1.21)
- But this did not translate into a greater remission rate nor a greater treatment response for the bright light group
Fish oils
- In two studies comparing omega-3 fish oil to placebo treatment, one found a significant decrease in depressive symptoms compared to controls (n=33, MD -4.70, 95% CI -7.82 to -1.58) but the other found no difference between the two groups (n=21) in terms of mean depression scores, treatment response or remission rates.
Conclusion
The authors conclude succinctly:
The evidence is inconclusive to allow us to make any recommendations for the treatment of antenatal depression.
This is because the trials:
were too small with non-generalisable samples.
They note that there is:
greater evidence and clinical experience with traditional treatments (pharmacotherapy and psychotherapy).

This review concludes with the usual call to action to improve the quality of CAM research
Of course, a lack of substantial evidence does not mean that these treatments don’t work, but if they are to be properly evaluated then the authors recommend that future research in this area will have to use:
- Standardised diagnostic criteria;
- Larger sample sizes;
- Proper blinding;
- The inclusion of proper placebo controls;
- Systematic evaluation of side effects; and
- Standardisation of dosage, potency and concentrations
Discussion
I’ll take up two points that have been raised in a previous Mental Elf post on CAM treatments by Caroline Tomes.
Don’t combine CAM therapies into huge reviews unless it makes sense to do so
Firstly, not all treatments outside of pharmacotherapy and psychotherapy should be lumped together. One group contains therapies emerging from improved understanding of the relationship between physical and mental health – including the role of circadian rhythms, and the interaction with the endocrine and inflammatory systems. Another group contains treatments that are underpinned by far more speculative and unproven theoretical systems and a disservice is done to the former group by conflation with the latter.
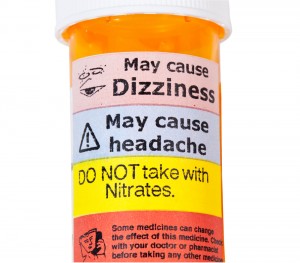
The side effects of mainstream drug treatments are fairly well understood, but unregulated CAM therapies are more of a minefield for patients
Don’t forget the potential harms of unregulated and untested therapies
Secondly, while it is clear from this review that there is no firm evidence for complementary treatments to displace conventional treatments for antenatal depression (and many other illnesses) they are generally used by doctors and patients as an adjunct, rather than a replacement. In this context, the important question is do the benefits outweigh the risks? To answer this we need not only to evaluate their efficacy, but also their side effects. Presumably, there is no downside to maternal massage but can we be as sure of the various chemicals proffered as nutraceuticals?
Further research will allow us to determine if any of the vast group of CAM therapies offer effective treatments for antenatal depression without the limitations of currently proven treatments.
Link
Dennis CL, Dowswell T. Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No.: CD006795. DOI: 10.1002/14651858.CD006795.pub3.
Tomes, C. CAM: Many of us are using it, despite poor evidence. Whats going on? The Mental Elf, 10 Oct 2013.

Is ‘natural’ better? Evidence for the efficacy of complementary therapies for antenatal depression: Can we enc… http://t.co/W8M7gdacjh
RT @Mental_Elf: Is ‘natural’ better? Evidence for complementary therapies for AND http://t.co/EYcLmQqzx0 < fascinating cc @Netmums
Is ‘natural’ better? Evidence for the efficacy of complementary therapies for antenatal depression http://t.co/ED162DlAn5 via @sharethis
Is ‘natural’ better?Evid for the efficacy of complementary therapies for antenatal depression http://t.co/Or0WcRgVNn Any thoughts @zeno001?
Via @pash22 @Mental_Elf : Is ‘natural’ better?Evid for the efficacy of CAM therapies for antenatal depression http://t.co/qIONiaFPge
@markhoro highlights a recent @cochranecollab review of complementary therapies for treating antenatal depression http://t.co/jzIcUmuEWS
@EdzardErnst We’d be interested to hear your thoughts on our blog about CAM & antenatal depression http://t.co/jzIcUmuEWS @markhoro
@Mental_Elf with side-effects & issues of combined meds, natural alternatives can play a huge part overall treatment for many people
Remedial maternal massage during pregnancy may help to reduce symptoms of antenatal depression http://t.co/jzIcUmuEWS
@Mental_Elf You write that they say greater evidence for pharmacotherapy? I’ve searched http://t.co/e6qMdhlN8b ‘antenatal depression’ no ev?
@wouterhavinga @Mental_Elf Pubmed/google scholar- there are papers on the risks of SSRIs (certianly not risk-free) and benefits in pregnancy
@NHSChoices #CochraneEvidence on CAM treatment for antenatal #depression blogged today by @Mental_Elf http://t.co/ejxRlA5Frw @CochranePCG
Read our blog on new #CochraneEvidence about complementary therapies for antenatal depression http://t.co/jzIcUmuEWS
Don’t miss: Is ‘natural’ better? Evidence for the efficacy of complementary therapies for antenatal depression http://t.co/jzIcUmuEWS
@Mental_Elf The other side of ris risk. How about an analysis of the risk of CAMS and Antidepressants in pregnancy? Complete picture needed.
Mental Elf: Is ‘natural’ better? Evidence for the efficacy of complementary therapies for antenatal depression http://t.co/ak7TOUBQaH
New from @Mental_Elf Is ‘natural’ better? Evidence for efficacy of complementary therapies for antenatal depression http://t.co/Sx32nWwT9K