
Herbal medicines often represent a cheaper alternative, or a low-cost complement, to standard pharmacotherapy. As a result, improved cost-effectiveness is often touted as a likely benefit of the use of complementary and alternative medicine (CAM).
Many, myself included, have been openly critical of CAM research, while others have suggested ways in which CAM research could be improved. As with studies of efficacy and effectiveness, there is a lack of good quality evidence regarding the cost-effectiveness of CAM-based interventions.
St. John’s wort (SJW) is a herbal medicine, most widely associated with the treatment of depression. Millions use it in the UK. A Cochrane review of its use for major depression has found it to be superior to placebo (Linde et al, 2008); a credential that few CAM treatments can claim. However, there remains a lack of evidence regarding the cost-effectiveness of the intervention.
A recent study by Solomon, Adams and Graves, published in the Journal of Affective Disorders (Solomon et al, 2013), attempts to begin filling the gap. We thought it well worth the elves having a look at this study and exploring the cost-effectiveness of St. John’s wort for the treatment of depression.
Methods
The study carries out a model-based economic evaluation of St. John’s wort compared with antidepressants for the treatment of acute mild to moderate depression. This approach synthesises data from different sources to answer questions about cost-effectiveness that have not previously been answered by prospective trials.
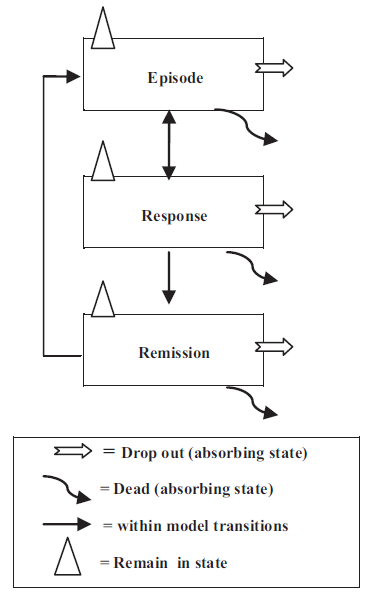
The study employs a Markov model, which requires that patients can be defined as being in one of a finite number of ‘states’, and that the probability of transition from one state to another is constant across all individuals within that state, regardless of their history. In this study the authors define 3 possible health states – depressive episode, response and remission – as shown in Fig. 1.
The model evaluates 3 possible courses of treatment; SJW, venlafaxine or sertraline. Each of these is associated with different probabilities of transition between the depression states and different costs.
The cost of SJW, venlafaxine and sertraline is 0.70, 1.35 and 0.75 $AUS per day respectively, and costs are estimated from the perspective of the national health provider.
The primary outcome is quality adjusted life years (QALYs), which are defined by the model states and are assumed constant across the treatment arms. The comparative benefit of treatment is defined by response rates, remission rates, relapse rates and adverse effects.
Results
Results indicate that SJW dominates – that is to say is cheaper and more effective than – antidepressants. Having carried out a probabilistic sensitivity analysis the authors assert that:
The decision maker can select SJW as the preferred or alternative treatment option with a high degree of confidence…
Limitations

It isn’t clear whether or not the study used data from comparable populations
Though the study is reasonably well reported it has a number of limitations.
- It’s possible that the study used some inappropriate data for its parameters. For example, response rates for venlafaxine are taken from a review including patients with mainly severe major depression, while the response rate for SJW appears to be based on an unpublished meta-analysis.
- Some assumptions also work in favour of SJW. For example, patients that discontinue then recommence treatment are assumed to require extended consultations with their GP, increasing the incremental cost of antidepressants.
- The design of the model also appears to be flawed. Individuals are allowed to ‘leave’ the model, in which case they become unobserved, and this could significantly bias the results.
- Furthermore, the model does not consider all possible treatment options. If we take a look at the NICE guidelines for depression, for example, we’ll see important roles for psychotherapy and cognitive behavioural therapy, as well as many alternative SSRIs and other classes of antidepressants. NICE guidelines do not explicitly recommend venlafaxine or sertraline.
- It’s also worth mentioning that the study received funding from the Complementary Healthcare Council of Australia.
Discussion

While it’s clear that the direct costs of SJW are lower, any indirect costs or savings to the health service remain unknown
Unfortunately this study is unable to identify, with any confidence, the likely incremental cost differences associated with the use of SJW. This is due in large part to the availability of data; the predictive validity of a model is wholly dependent on the availability of good data. While we know that the direct cost of SJW is lower than that for traditional antidepressants, there are no data available regarding the possible indirect costs of SJW. As such, the model must depend on inferences and assumptions about service use. These questions can only be answered by a prospective trial-based cost-effectiveness analysis.
It is reasonable to expect that the model used in this study, employing different assumptions, could produce entirely contradictory results. This is because the model is not comprehensive. Not only are there many other antidepressants aside from the two considered here, and non-pharmaceutical therapies, but there is also a wide array of SJW products. There are also many other relevant service use parameters that could have been included, such as inpatient care or contacts with community mental health teams, which could substantially alter the results.
Though no model can ever be definitive or entirely depended upon for policy decisions, there remains scope for a more comprehensive modelling study of the cost-effectiveness of SJW compared with alternative lines of treatment. Such a model would be greatly enhanced by a prospective trial of the cost-effectiveness of SJW, which could thoroughly capture the direct and indirect costs of treatment. Hopefully this is something on which the elves can report in the future.
Links
Solomon, D., Adams, J. and Graves, N. Economic evaluation of St. John’s wort (Hypericum perforatum) for the treatment of mild to moderate depression. Journal of Affective Disorders 2013; 148: 228-234. [PubMed]
Linde K, Berner MM, Kriston L. St John’s wort for major depression. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD000448. DOI: 10.1002/14651858.CD000448.pub3.
Depression in adults. NICE Clinical Guideline 90. National Institute for Health and Clinical Excellence, 2009.
Sampson, C.J., Whitehurst, D.G. and Street, A. Do patients registered with CAM-trained GPs really use fewer health care resources and live longer? A response to Kooreman and Baars. The European Journal of Health Economics 2013; 14(4): 703-705. [PubMed] [RePEc]
Solomon, D., Ford, E., Adams, J. and Graves, N. Potential of St John’s Wort for the treatment of depression: the economic perspective. Australian and New Zealand Journal of Psychiatry 2011; 45(2): 123-130. [PubMed]
Tomes, C. CAM: Many of us are using it, despite poor evidence. Whats going on? The Mental Elf, 10 Oct 2013.

@ChrisSampson87 blogs about a recent economic evaluation of St. John’s wort for depression http://t.co/GwFZzbuA1N
New blog post by me today on The Mental Elf, looking at the cost-effectiveness of St. John’s Wort for depression http://t.co/52eklNXqVC
Today’s blog compares the cost effectiveness of St John’s wort, venlafaxine & sertraline for depression http://t.co/GwFZzbuA1N
@Mental_Elf Sertraline I can see where there would be medical similarities – but Venlafaxine at higher doses is Norad.. & Dopaminergic
@MrMcTheatre Yes @ChrisSampson87 points out in his blog that other comparative treatments would have been useful http://t.co/GwFZzbuA1N
@Mental_Elf @ChrisSampson87 Ah. Sorry – should’ve read it properly :^\
@Mental_Elf @MagsyWagsyMeg thought the above tweet would interest you.
Cost-effectiveness of St John’s wort for treatment of depression http://t.co/C9lxwb9hg3 via @Mental_Elf:
St John’s wort is more effective than placebo for depression, but its cost-effectiveness remains uncertain http://t.co/GwFZzbuA1N
In case you missed it earlier: Cost-effectiveness of St John’s wort for treatment of depression http://t.co/GwFZzbuA1N
Mental Elf: Cost-effectiveness of St John’s wort for treatment of depression http://t.co/ChLuUURB2I
New from @Mental_Elf Cost-effectiveness of St John’s wort for treatment of #depression http://t.co/vIRcvCIh0P
Great @Mental_Elf analysis of effectiveness of St Johns Wort for #depression. Vexing methodological issues abound! http://t.co/H7Um7NrmDT
Studie zu Johanniskraut bei #Depressionen: Wirksam und günstig, aber einige Fragen bleiben offen http://t.co/qz0OFBOtUV via @Mental_Elf
Cost-effectiveness of St John’s wort for treatment of depression http://t.co/W2A8N2eyDd via @sharethis