
Depression is a multifaceted, complex condition and is a leading cause of disability worldwide. The pattern and severity of symptoms and the biological mechanisms of depression vary greatly between individuals (Buch and Liston, 2020). This variability in diagnosis and the lack of identified biomarkers may be one of the reasons why about a third of individuals with depression are resistant to antidepressants (Akil et al., 2018), posing significant barriers toward personalised interventions.
Compelling evidence shows that dysfunction of the immune system, particularly elevated levels of blood cytokines and acute phase proteins contribute to the development of depression (Khandaker et al., 2014). However, studies testing anti-inflammatory agents in randomised trials have found mixed results (Jeppesen et al., 2020). It is becoming increasingly apparent that immune dysregulation is not present in all individuals with depression, but only in a subset (Khandaker et al., 2018). This may explain why immunotherapy may not work for all patients. There is therefore a pressing need to identify immune biomarkers with diagnostic potential to help select individuals for personalised immunotherapy trials with successful response rates.
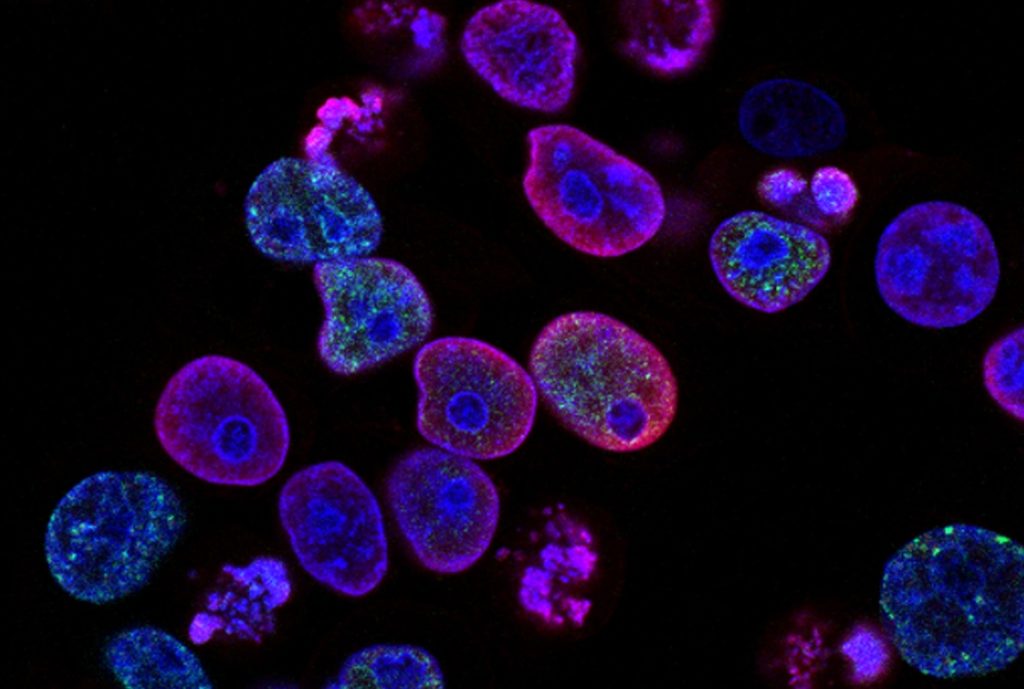
White blood cells (WBCs) are part of the body’s immune system. Our immune system can be divided into two (interacting) arms:
- The innate arm is the body’s first line of defence, responding quickly but more generally to pathogens, without an immunological memory of previous responses
- The adaptive arm is slower but highly specific to pathogens, and is characterised by memory.
The general aim of the immune system is to defend our body against pathogens or tissue damage, but dysfunction in the innate or adaptive immune systems can contribute to physical and neuroimmune diseases (Corsi-Zuelli & Deakin, 2021). Studying this closer could help us to understand the nature of immune dysregulation in depression and help us to identify biomarkers of the illness. Therefore, Foley et al. (2022) performed a systematic review and meta-analysis of peripheral immune cells in depression compared with controls, aiming to provide state-of-the-art evidence that will be useful for future immunotherapy trials.

Depression is a multifaceted condition with great variability in symptoms, severity, and response to treatment. Immune cells could be promising biomarkers for personalised interventions, but more research is needed.
Methods
Following PRISMA guidelines, two databases were searched in April 2022 for all cohort or case-control studies which compared the immune phenotype of non-immunocompromised adults with either current depression or with no lifetime history of psychiatric illness. Only studies using flow cytometry or related techniques to count cells per group were included.
Two authors independently performed the search strategy, applied the inclusion and exclusion criteria, extracted data, and assessed study quality. Hand-searching was also used to complement the electronic search. Any inconsistencies were resolved by discussion with a senior author.
The main outcome was absolute cell count and/or relative percentage of blood immune cells in individuals with depression and controls. Study quality was assessed using the Newcastle-Ottawa Scale (NOS).
The authors calculated the standard mean difference (SMD) of absolute cell counts and relative percentages using an inverse variance method and quantitative random-effect meta-analysis. Heterogeneity was measured by the I2 statistic and publication bias by Egger’s test. Sensitivity analyses were also performed by excluding any extreme outliers.
Results
The initial search identified 934 studies after removing duplicates. From these, 33 met the inclusion criteria, and 27 included sufficient data for meta-analysis. All studies were of reasonable quality (NOS ≥4 out of a maximum score of eight).
Compared with controls, individuals with depression presented increased mean of absolute cell counts for the following cellular populations:
| Cellular
population |
No of
studies |
Sample
size |
Results
(MDD vs HC) |
Statistics
(SDM; I2) |
| WBC count | 7 | MDD=163; HC=105 | ^ | 1.07; 64% |
| Myeloid cells | ||||
| Granulocytes | 2 | MDD=34; HC=32 | ^ | 2.07; 0% |
| Neutrophils | 4 | MDD=282; HC=117 | ^ | 0.91; 82% |
| Monocytes (CD14+) | 7 | MDD=191; HC=141 | ^ | 0.60; 66% |
| Lymphoid cells | ||||
| T CD4+ | 11 | MDD=465; HC=307 | ^ | 0.30; 0% |
| NK cells (CD16+CD56+) | 11 | MDD=291; HC=277 | ^ | 1.23; 95% |
| B cells (CD19+)* | 11 | MDD=468; HC=305 | ^ | 0.30; 56% |
| Activated T cells (CD25+) | 8 | MDD=233; HC=169 | ^ | 0.41; 0% |
| Activated T cells (CD3+HLADR+) | 8 | MDD=233; HC=169 | ^ | 0.50; 21% |
| *After removing one extreme outlier | ||||
| MDD= individuals with major depressive disorder; HC = healthy controls | ||||
For total lymphocytes and other T cell subtypes (T CD3+, T CD8+, CD4+/CD8+ ratio, and naïve T cells CD45RA+) there were no differences in the mean of absolute cell counts in individuals with depression compared with controls.
In addition, there were no studies on absolute cell counts for Th1, Th2, Th17, regulatory T cells (Tregs) or memory T cells (CD45RO+/CD45RA-).
Bias assessment
Publication bias was found for two cellular subsets: mean absolute counts of total lymphocytes and relative percentage of cytotoxic T cells.
The results suggest that both innate and adaptive immune cells are implicated in the development of depression.
Conclusions
The authors concluded that,
depression is associated with alterations in several myeloid and lymphoid cells, including increased mean absolute counts of total WBC, granulocytes, neutrophils, monocytes, CD4+ helper T cells, NK cells, CD19+ B cells, and CD25+ and CD3+ HLADR+ activated T cells, but decreased relative percentage of lymphocytes, Th1, and Th2 cells.
The findings suggest the involvement of both innate and adaptive immune cells in the development of depression.
Identifying dysfunctional immune cell subsets could help select patients with depression who show signs of immune dysfunction for future immunotherapy trials. However, further studies are needed to understand causality and how immune cell dysfunction relates to cytokine and neurotransmitter dysregulation.
This is one of the first meta-analyses to investigate the peripheral blood cellular immunophenotype of depression, with findings suggesting that peripheral blood immune cells could serve as biomarkers for personalised treatments for depression.
Strengths and limitations
Strengths included:
- A large number of cases (n = 1,286) and controls (n = 991)
- Assessing the quality of studies using a validated scale and publication bias by visual inspection of funnel plots and Egger’s test
- Rigorous inclusion criteria, including only depressed cases defined using validated scales and to ensure controls had no lifetime history of psychiatric illness
- Investigating innate immune cells (e.g., monocytes), which had been previously implicated in the development of depression, in addition to adaptive immune cells, such as T cells, which have received less attention so far.
However, data on adaptive immune cells were scarce to draw firm conclusions, particularly for T cell subtypes such as Th1, Th2, Th17 and Tregs. The results suggested decreased relative percentage of total lymphocytes, Th1 and Th2 cells, and no differences for Th17 or Tregs. Nonetheless, data on absolute counts of T cell subsets were not available. This is an important limitation because, as acknowledged by the authors:
(…) relative percentages are a holistic representation of the immune landscape at the time of sampling. Unlike total cell count, change in relative percentage of one cell type can be influenced by changes in another cell type(s).
Therefore, the decreased relative percentages of T cell subsets could merely reflect increased absolute numbers of other cellular populations. However, an important strength of the study is that the authors primarily focused their results on mean absolute cell count, in line with standard immunology practice.
Limitations include:
- The fact that the study and its protocol were not registered prior to analysis
- Most data came from cross-sectional studies prone to selection bias
- There was a bias towards mean absolute levels of total lymphocyte counts and relative parentages of CD8+ T cells
- Heterogeneity across studies remained high after removing outliers, particularly for WBC, neutrophils, monocytes, and NK cells. This likely reflects differences in studies’ methods
- Certain cellular subsets contained very few studies
- The effect of confounding, especially medication, needs further investigation.
Hence, it is not possible to infer causality, as reverse causation and confounding cannot be ruled out, remaining unknown whether changes are cause or consequence of illness, which will require genetic approaches such as Mendelian Randomisation.

This comprehensive meta-analysis is the first of its kind, providing state-of-the-art information on cellular immunophenotype of depression, advancing our current knowledge for future selective immunotherapy trials.
Implications for practice
The molecular heterogeneity of depression may explain the conflicting evidence of immunotherapy trials. To increase success rates in future trials, we urgently need to identify biomarkers to help select patients with immune dysfunction for future personalised trials. The comprehensive findings provided by Foley et al. (2022) are persuasive in convincing us that it is time to aggregate data on immune cell phenotyping to cytokine measurement to better understand immune mechanisms of depression and identify reliable biomarkers with clinical potential.
One important consideration that can be drawn is that immune phenotyping data is much less available than cytokine research. Despite that, the findings suggest that mechanisms are unlikely solely caused by innate immune cells such as monocytes; instead, immune dysfunction expands to the adaptive immune system, including T cells and their subtypes. This observation is consistent with the view that there is no “monolithic” immunophenotype of depression (Felger and Miller, 2020). The involvement of T cells is particularly attractive, given the identification of protective subtypes in the healthy human brain parenchyma and their intimate connection with astrocytes and microglia, as I reviewed recently with colleagues (Corsi-Zuelli & Deakin, 2021; Corsi-Zuelli et al., 2021).
It is still unclear how dysfunctional peripheral immune cells could contribute to morphological, neurochemical, and functional changes in the central nervous system or how they could causally influence the risk of depression. To answer some of these questions, we need longitudinal studies conducted with drug-naïve or minimally treated patients using sophisticated immunophenotyping methods to distinguish immune cell subsets and unravel their relevance to specific symptom profiles. Data on absolute numbers or percentages are insufficient to measure immune cells’ ability to release or inhibit cytokines; therefore, in vitro studies are required to test immune cells’ functional capacity. Imaging methods could help to assess the relationship between brain, glial, and neurotransmitter changes with circulating immune cells.

Comprehensive immunophenotyping and cytokine measurement will help move us beyond correlations towards understanding causation and being able to develop person-specific immune interventions.
Statement of interests
Fabiana Corsi-Zuelli is a PhD student at the Ribeirão Preto Medical School at the University of São Paulo, funded by the São Paulo Research Foundation (FAPESP; Fellowship 21/07448-3 and 19/13229-2).
Links
Primary paper
Foley, É. M., Parkinson, J. T., Mitchell, R. E., Turner, L., & Khandaker, G. M. (2023). Peripheral blood cellular immunophenotype in depression: a systematic review and meta-analysis. Molecular Psychiatry, 28(3), 1004–1019.
Other references
Akil, H., Gordon, J., Hen, R., Javitch, J., Mayberg, H., McEwen, B., … & Nestler, E. J. (2018). Treatment resistant depression: a multi-scale, systems biology approach. Neuroscience & Biobehavioral Reviews, 84, 272-288.
Buch, A. M., & Liston, C. (2021). Dissecting diagnostic heterogeneity in depression by integrating neuroimaging and genetics. Neuropsychopharmacology, 46(1), 156-175.
Corsi-Zuelli, F., & Deakin, B. (2021). Impaired regulatory T cell control of astroglial overdrive and microglial pruning in schizophrenia. Neuroscience & Biobehavioral Reviews, 125, 637-653.
Corsi-Zuelli, F., Deakin, B., De Lima, M. H. F., Qureshi, O., Barnes, N. M., Upthegrove, R., … & Del-Ben, C. M. (2021). T regulatory cells as a potential therapeutic target in psychosis? Current challenges and future perspectives. Brain, Behavior, & Immunity – Health, 17, 100330.
Felger, J. C., & Miller, A. H. (2020). Identifying immunophenotypes of inflammation in depression: dismantling the monolith. Biological Psychiatry, 88(2), 136-138.
Jeppesen, R., Christensen, R. H., Pedersen, E. M., Nordentoft, M., Hjorthøj, C., Köhler-Forsberg, O., & Benros, M. E. (2020). Efficacy and safety of anti-inflammatory agents in treatment of psychotic disorders–A comprehensive systematic review and meta-analysis. Brain, Behavior, and Immunity, 90, 364-380.
Kenney-Williams, P. (2016). Depression. The Mental Elf.
Khandaker, G. M., Pearson, R. M., Zammit, S., Lewis, G., & Jones, P. B. (2014). Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life: a population-based longitudinal study. JAMA Psychiatry, 71(10), 1121-1128.
Khandaker, G. M., Oltean, B. P., Kaser, M., Dibben, C. R., Ramana, R., Jadon, D. R., … & Jones, P. B. (2018). Protocol for the insight study: a randomised controlled trial of single-dose tocilizumab in patients with depression and low-grade inflammation. BMJ Open, 8(9), e025333.
Photo credits
- Photo by National Cancer Institute on Unsplash
- Photo by Pawel Czerwinski on Unsplash
- Photo by National Cancer Institute on Unsplash
- Photo by Julia Koblitz on Unsplash
- Photo by Daniel Gonzalez on Unsplash
- Photo by Prateek Katyal on Unsplash
