
A major challenge in the treatment of depression is that only a proportion of people respond to the first treatment they try. For example, with antidepressants only 40% of people will see their symptoms fall to a level that can be considered a recovery. Trying further treatments after the first one does not work can be effective (STAR-D), but it leads to a substantial delay in people feeling better.
While severity of depression does predict response, there is no current way of predicting who will respond to a specific treatment. Whether to go for an antidepressant or a course of psychotherapy is a crucial day to day decision made by both sufferers and professionals. Being able to predict who responds, and perhaps more importantly who will not, would be a major advance in reducing the burden of depression. Other branches of medicine rely heavily on using pre-treatment tests to determine the best treatment for an individual and replicating this in mental health problems would be extremely helpful.

Depression is associated with changes in brain structure and function
Brain imaging has the potential to be a tool that could predict response. As we have discussed before on the mental elf blog, depression is associated with changes in brain structure and function. Previous studies have shown that recovery is also associated with changes on brain imaging but this has not been tied to a specific treatment.
Methods
Researchers in America decided to use Positron Emission Tomography (PET) scanning to try and find out who would respond better to an antidepressant (escitalopram) or cognitive behavioural therapy (CBT) (McGrath, 2013). PET scanning uses a radioactive marker to measure the blood flow around the brain, a proxy measure for brain activity. In this study participants were asked to lie in the scanner for about 40 minutes and were not given any task to do during the scan. The scan occurred before any treatment was given and after a break from any previous treatment. 16 sessions of CBT were compared with 20-40mg of escitalopram, broadly in line with NICE guidance in the UK.
People who participated in the study had:
- A primary diagnosis of major depression
- A score of >18 on the Hamilton Depression Rating Scale (HDRS). This equates to an episode of at least moderate severity
- No suicidal ideation
- No serious physical health conditions eg chronic pain
- No current harmful use of any substances
- No history of a failure to respond to either of the interventions used in the study
In order to compare people who saw a recovery of their depressive episode (HDRS falling to below 7) to those who did not respond (<30% fall in the HDRS), people who saw only a partial response to the treatment (>30% fall but not to <7 on the HDRS) were not included in the primary analysis. This meant that of the 82 people who were randomised at the start of the study, only 38 people were included in this paper. The rate of recovery was the similar in the antidepressant group (12/30, 40%) and CBT (12/33, 36%), as was the rate of non-response (antidepressant 6/30 20%, CBT 9/33 27%).
Results

The researchers who conducted this study could have done more to minimise the possibility of false positives
The researchers were looking for areas in the brain where the level of blood flow at baseline was different in those who responded to CBT versus escitalopram. Due to the problem of multiple comparisons in brain image analysis the setting of the significance level is crucial in trying to understand the importance of the results. Researchers try to match clinical or behavioural factors to thousands of small areas of the brain (voxels). That means that they need to be very careful about how to reduce the risk of false positives. In this study this was not done as robustly as it could have been done. Using a level of significance that meant there was a high likelihood of false positives they identified 6 regions of the brain. On further analysis only one area was potentially showing a more robust effect: the right insula. In this area:
- Responders to escitalopram had a higher level of blood flow than non-responders
- Responders to CBT had a lower level of blood flow than non-responders
Conclusions
The researchers concluded that the:
data suggests that insula metabolism alone may serve as a pretreatment biomarker to guide initial treatment selection
but that “prospective studies are needed to further evaluate” their findings.
Summary
-
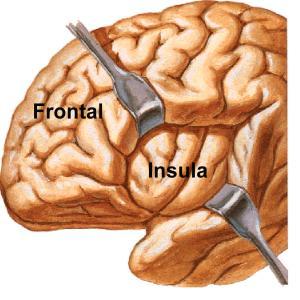
Changes to the function of the insula have been consistently implicated in depression at all stages of the illness
This study provides a proof of the concept that brain imaging could be used to differentiate subsequent response to different treatments.
- Sharp-eyed Mental Elf regulars will have spotted that the insula has been discussed before in relation to depression. It is part of emotion regulating networks in the brain and changes to its function have been consistently implicated in depression at all stages of the illness.
- The participants in this study were very tightly selected and stratified, and the results are difficult to generalise to clinical practice in the UK.
- Whether people would be willing to have a routine scan that involves a small dose of radiation is unclear.
- Unfortunately, in contrast to some media reports of this article (Wired, 2013), it does not mean that brain scans will be used to determine treatment any time soon.
- Exciting pilot study, but more research please.
Links
McGrath CL, Kelley ME, Holtzheimer PE, et al. Toward a Neuroimaging Treatment Selection Biomarker for Major Depressive Disorder. JAMA Psychiatry. 2013;():1-9. doi:10.1001/jamapsychiatry.2013.143. [Abstract]
Study: brain scans indicate best individual treatment for depression. Wired.co.uk, 13 June 2013.


@Mental_Elf This is interesting. CBT does not work for everyone and certain medication might work on some people, but not others.
“@Mental_Elf: Can brain imaging help predict who will respond to CBT versus antidepressants? http://t.co/XCCKtyni0W” #ffs
@Mental_Elf excellent blog and really interesting and fascinating study
@andrewwatson28 explains why brain scans won’t be used to determine depression treatment any time soon http://t.co/VcKB7TdJu4
“@Mental_Elf: Can brain imaging help predict who will respond to CBT versus antidepressants? http://t.co/HyucRQfmfG” hopefully
@Mental_Elf Why the constant focus on CBT … Other therapies are available! I use person centred successfully with clients.
@WiredUK We disagree w/ yr reporting of new research. Your blog: http://t.co/HZSyudKUa8 Our blog: http://t.co/VcKB7TdJu4 Thoughts?
New research shows how PET scanning may be used in future to help steer depression treatment decisions http://t.co/VcKB7TdJu4
@Mental_Elf Do you have any current research on SAD? Curious.
@andrewwatson28 blogs on @JAMAPsych Toward a Neuroimaging Treatment Selection Biomarker for Depression http://t.co/VcKB7TdJu4
In case you missed it: Can brain imaging help predict who will respond to CBT versus antidepressants? http://t.co/VcKB7TdJu4
@Mental_Elf It could@well@be the way forward.
@Mental_Elf @drinksinthedark however, the whole ethos around the IAPT programme & CBT was cost effectiveness so likelihood of using it slim
@psychjunkie3 @Mental_Elf I guess it could take off in the US though (or even here with privatisation).
Can #brainimaging help predict who will respond to #CBT versus #antidepressants? http://t.co/B6AFRiaC3Z via @Mental_Elf
Mental Elf: Can brain imaging help predict who will respond to CBT versus antidepressants? http://t.co/V6hpCHdYxU
Great blog. Thought provoking according to recent scans. I’d be very keen to know if these findings would be “limited to CBT”