
Functional neurological disorder (conversion disorder) is a common cause of disabling neurological symptoms. Despite its frequency in normal medical practice, it has occupied an unenviable twilight zone in terms of understanding its pathophysiology.
The most pervasive idea has been that traumatic life events, in particular childhood trauma, are causal. There is a logical consequence of this idea, encapsulated in the theory of conversion disorder put forward by Breuer and Freud, that treatment of this disorder rests on the uncovering, exploration and resolution of the underlying trauma, through which symptoms will disappear (Freud and Breuer, 1978).
Over the past 15 years there has been increasing interest in functional neurological disorder (FND), and with it a questioning of the relevance of traumatic life events. Within DSM 5, changes to diagnostic criteria demoted the presence of a psychological formulation as a supporting but not essential criterion, and instead emphasis was placed on the demonstration of specific features on history and examination that were positive features of functional neurological disorder.
Against this background, Ludwig et al performed a meta-analysis of studies that had looked at the association between adverse life events and functional neurological disorder.

A new meta-analysis published today explores the association between adverse life events and functional neurological disorder.
Methods
The authors searched for case control studies that recorded life events in patients with functional neurological disorder/conversion disorder that were indexed in PubMed and ScienceDirect between 1965 and 2016. They also searched reference lists for eligible studies and reviews.
They included studies with more than 10 subjects where they included comparison between functional neurological disorder patients and at least one control population. They performed standard ratings of study quality and calculated odds ratios and population attribution factors (PAF), which is a measure of the contribution of a risk factor to a disease at a population rather than individual level.
Results
The authors identified 34 eligible studies with a total of 1,405 patients.
Rates of childhood stressors
| Functional neurological disorder | Controls | Odds ratio (95% confidence interval) |
|
| Emotional neglect |
49% | 20% | 5·6 (2·4 to 13.1) |
| Sexual abuse |
24% | 10% | 3·3 (2·2 to 4.8) |
| Physical abuse |
30% | 12% | 3·9 (2·2 to 7.2) |
Stressful life events preceding onset were also more common in patients with FND when compared with controls.
However, a notable proportion of patients did not appear to have either childhood maltreatment or recent stressful life events.
The quality of studies was low-moderate.
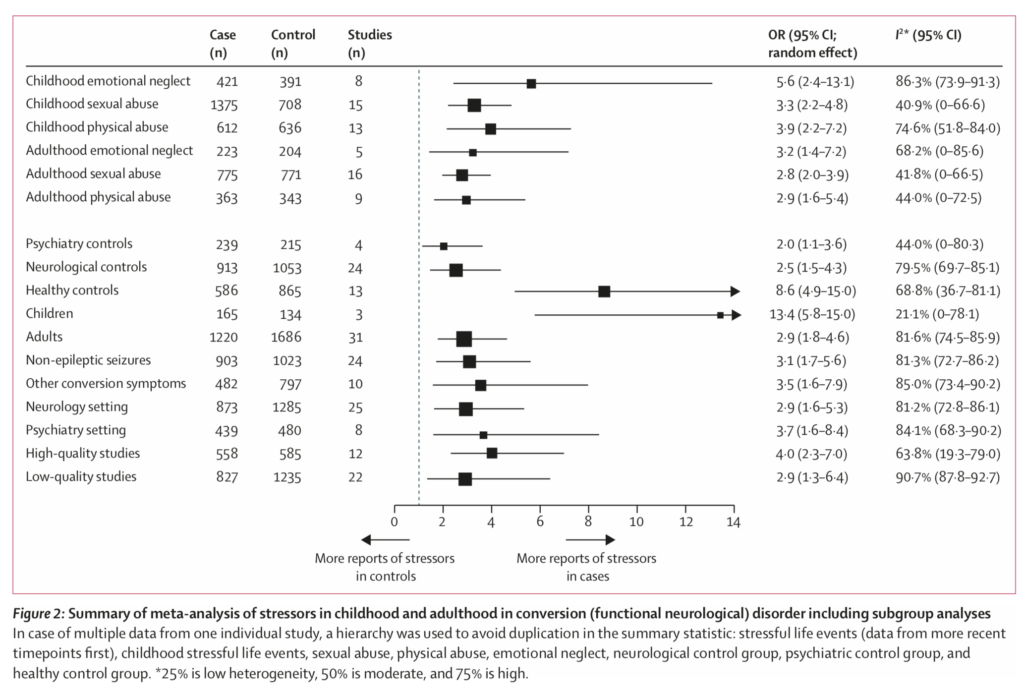
This meta-analysis found that “stressful life events and maltreatment were substantially more common in people with functional neurological disorder than in healthy controls and patient controls”.
Conclusions
The analysis suggests that adverse experiences both in childhood and adulthood are associated with the development of functional neurological disorder. However, there was considerable heterogeneity both in the nature of the adverse experiences and also if they occurred at all, with a notable proportion of people reporting no such events.
Strengths and limitations
The main limitations relate to the quality of the studies sampled for the meta-analysis. Multiple methods were used to assess life events and childhood trauma, and of course all such assessments were retrospective. In studies with arguably more rigorous methods of life events ascertainment, a higher rate of adverse life events prior to onset of symptoms was found.

There was considerable heterogeneity across studies, both in the nature of the adverse experiences and also if they occurred at all, with a notable proportion of people reporting no such events.
Implications for practice
The idea that adverse childhood and later experiences have an influence on risk of developing (mental) illness is not a new one. For example, rates of adverse events in people with schizophrenia and depression are high. However, in functional neurological disorder these events have seemed to morph from risk factors/associations to the cause. This has had a number of negative consequences:
- Firstly, it suggests that diagnosis requires the presence of these factors. Under previous iterations of DSM it was not possible to make the diagnosis of conversion disorder without there being a “psychological formulation”. This illogical situation led to some patients being passed between neurologists and psychiatrists in an anti-therapeutic game of ping pong, with neurologists declaring the symptoms to be “non-organic” and psychiatrists declaring the patient to be “psychologically well”.
- Second, it suggests that the only treatment that will help is one that is directed towards the uncovering and resolution of underlying traumatic experiences. In contrast, treatments that work at the level of how symptoms are produced, delivered by psychologists, physiotherapists, occupational therapists were not prioritised or viewed as legitimate or valuable.
- Third, it subsumes the reality of the physical symptoms experienced by the patient within another phenomenon (past trauma) as if the symptoms are not a thing in their own right, and, in a sense, are not real.
Importantly, this paper is not an excuse to throw out the idea of an association between adverse life events and functional neurological disorder; rather it calls for us to consider the mechanism of the association and to understand how this should influence treatment (and even prevention). It supports the rebalancing of diagnostic approach, explanation and treatment that has been promoted in recent times and (at the very least) supports allowing the disorder to be classified in ICD-11 in the neurology and psychiatry sections. However, as the authors point out, the hope would be that in the end there would be a merging of these categories to one that recognises the indivisible nature of brain and mind.

Importantly, this paper is not an excuse to throw out the idea of an association between adverse life events and functional neurological disorder; rather it calls for us to consider the mechanism of the association and to understand how this should influence treatment (and even prevention).
Conflicts of interest
I was a reviewer for the paper and have previously published papers with several of the authors.
Links
Primary paper
Ludwig L, Pasman JA, Nicholson T, Aybek S, David AS, Tuck S, Kanaan RA, Roelofs K, Carson A, Stone J. (2018) Stressful life events and maltreatment in conversion (functional neurological) disorder: systematic review and meta-analysis of case-control studies. The Lancet Psychiatry 2018
Commentary. The Lancet Psychiatry 2018
Other references
Freud S, Breuer J. (1978) Studies in hysteria. Harmonsworth, UK: Penguin; 1978.

Is there even any positive (and not outdated) proof of FND? As far as I’m concerned, diagnosis revolves around a) finding no positive signs of disease, b) disbelieving patient testimony and then c) tricking patients into doing things that the practitioner thinks they shouldn’t be able to do if they had a true neurological condition (even though these things are largely based on antiquated understandings of how the brain works). It just seems like a very problematic diagnosis with very shaky evidence. Science requires proof, not an undergrad literary thesis on the imaginary effects of the mind on the body.
Spot on.
Couldn’t agree more.
I have just been diagnosed with FND by a neurologist who was very clear that it’s a real diagnosis with real symptoms, and a lot of the info I’ve found has stressed that it’s supposed to be a positive diagnosis not one of exclusion.
I think I feel ok about it because it was explained well and sadly sometimes it’s not.
This is a really interesting read. My husband has recently being diagnosed with FND after being seen for just 30mins. He has no past Trauma and so has struggled to understand a diagnosis that doesn’t seem to fit into a mental health category for him. It is good to see that work is still being done to investigate this illness.
In psychiatry nothing is “off the table”, and in neurology nothing in “on the table” unless there is necessity. The dilema being that apples falling from different trees, show the exact same bruising, yet it must relate to how they are grown somehow… unlikely?