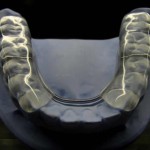
Temporomandibular disorders (TMDs) can affect the temporomandibular joint (TMJ) the muscles of mastication or both. A range of factors have been related to TMDs , occlusion, trauma, deep pain stimulus, parafunctional activities and psychological factors, such as anxiety, depression and stress . It has also been suggested that postural problems related to the head and [read the full story…]