Following tooth loss, it may not be possible to restore the dentition with a fixed prosthesis due to issues with the size and distribution of the saddle area/s, abutment distribution and bone quantity/quality. This problem can be partly resolved using a removable partial denture (RPD), but good retention and stability may be challenging to achieve for the same reasons as stated above. This paper sets out to see if the use of strategically placed osseointegrated dental implants stabilising removable partial dentures presented better predictability for the rehabilitation of partially edentulous patients than conventional removable partial dentures (RPDs).
Methods
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines and registered the protocol on PROSPERO. The primary outcome was implant survival rate, while the secondary outcomes were marginal bone loss and patient-reported outcome measures (PROM). The eligible studies were randomised controlled trials (RCTs) and prospective studies published in English. Two independent authors conducted an electronic search of the MEDLINE/PubMed, EMBASE, Web of Science, and Cochrane Library databases for articles published up to December 2020; hand searching was carried out in the journals, Clinical Implant Dentistry and Related Research, Clinical Oral Implants Research, Implant Dentistry, International Journal of Oral and Maxillofacial Implants, Inter- national Journal of Oral and Maxillofacial Surgery, International Journal of Prosthodontics, Journal of Clinical Periodontology, Journal of Dentistry, Journal of Oral and Maxillofacial Surgery, Journal of Oral Implantology, Journal of Oral Rehabilitation, Journal of Prosthodontics, and The Journal of Prosthetic Dentistry with www.opengrey.eu being searched for non-peer reviewed literature. The risk of bias was assessed using the Cochrane Collaborations tool for RCTs and the Newcastle-Ottawa Scale for non-RCT studies. Meta-analysis was undertaken using the software package “meta” in R.
Results
- Sixteen studies were included, 3 were RCTs, and 13 had a prospective design.
- A total of 334 participants and a mean age of 58 years received 581 dental implants (475 conventional and 106 mini-implants).
- The mean follow-up duration was 36.8 months.
- RCT studies exhibited a low risk of bias for most domains, while most non-RCT studies were classified as good quality.
- Meta-analysis indicated a high proportion of implant survival rates of 3% (95%CI: 2% to 5%) and a low mean raw score of marginal bone loss of 0.98 mm (95%CI: 0.61 to 1.36 mm).
- A variety of PROMs evaluation tools were used. These were the oral health-related quality of life (OHRQoL), the oral health impact profile (OHIP-49), the short-form health survey (SF-36), a visual analogue scale (VAS), and a patient satisfaction questionnaire. Compared with conventional RPDs the ISRPDs, subjectively improved patient quality of life and mastication.
Conclusions
The author concluded: –
Implant-supported RPDs exhibited high implant survival rates and acceptable bone loss with improvement in patients’ quality of life and satisfaction when compared with conventional RPDs. Therefore, they can be considered suitable for the rehabilitation of partially edentulous patients.
Comments
This review followed standard preregistration and systematic review protocols but excluded non-English studies, which may have missed some relevant studies. However, the results need to be interpreted with a high degree of caution for the reasons stated below.
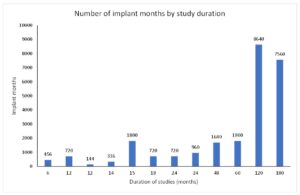
An interesting observation from these meta-analyses is the problem of combining a small number of studies with high variance. The authors stated in their methods section that if there was no significant heterogeneity between the studies, a fixed-effects (common-effects) meta-analysis would be performed. The authors mention that this systematic review was limited by different follow-up periods that ‘may have’ directly influenced the heterogeneity and results but still used a fixed-effects model. This limitation of heterogeneity could have been overcome by reporting the variance and uncertainty rather than just the point estimate and 95% confidence intervals. To demonstrate this, I have used their primary outcome data for implant failure. The histogram below indicates that the implant survival data has a left-sided skew, so it would be more appropriate to use the weighted median plus range when describing follow-up duration. In this case, the median study duration was 60 months (Range: 6 to 180 months) rather than the mean 36.8 months published. (Figure 1.)
Figure 1
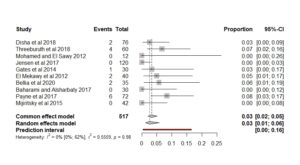
The second point was the authors used a fixed-effects meta-analysis contradicting their methods section. A fixed-effects model makes sense if the studies are functionally identical. In this case, they are not as there are variances in duration, implant type and location of placement. (Borenstein et al., 2011). The meta-analysis and forest plot have been reproduced below using metaprop in R. (Version 5.1-0) to demonstrate a couple of interesting points. (Figure 2.)
Figure 2
Firstly, there is very little difference between the fixed-effects and random-effects models, except the confidence interval for the random effects has 2% more spread. In the author’s version, the heterogeneity was I2 = 48%, and in this meta-analysis, we have an I2 = 0%. This point estimate value of zero can be highly misleading and is caused by combining a small number of studies that have wide confidence intervals. To correct this bias, von Hippel recommends reporting the 95% confidence interval in addition to the point estimate I2. In this case, the 95% confidence interval ranges from 0 to 62%, indicating a wide degree of uncertainty. (von Hippel, 2015).
The final point relates to the addition of prediction intervals into future meta-analyses. The standard point estimate and confidence interval presented in a metanalysis do not inform the researcher as to how the true effects are distributed about the point estimate. This is important to understand when predicting the survival rate for future implant placement under RPDs in this case. (Borestein et al. 2011)
To more accurately represent the high degree of variability in this updated meta-analysis using the prediction interval, the implant failure summary estimate data could be presented as:
Over a period ranging from 6 months to 180 months, the mean failure rate was 3% (95%CI: 1% to 6%) with a 95% prediction interval of true future failures of 0% to 16%.
Links
Primary paper
Lemos, C. A. A., Nunes, R. G., Santiago-Junior, J. F., et al. 2021. Are Implant-Supported Removable Partial Dentures a Suitable Treatment for Partially Edentulous Patients? A Systematic Review and Meta-Analysis. J Prosthet Dent. 2021 Jul 27:S0022-3913(21)00334-6. doi: 10.1016/j.prosdent.2021.06.017. Epub ahead of print. PMID: 34330529.
Other references
Borenstein, M., Hedges, L. V., Higgins, J. P., et al. 2011. Fixed-Effects Versus Random-Effects Models. Introduction to Meta-Analysis. John Wiley & Sons.
Borenstein, M., Hedges, L. V., Higgins, J. P., et al. 2011. Prediction intervals. Introduction to Meta-Analysis. John Wiley & Sons.
von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015 Apr 14;15:35. doi: 10.1186/s12874-015-0024-z. PMID: 25880989; PMCID: PMC4410499.