We are having a tweet chat at 8-9pm BST on Monday 11th July to discuss how best to support oral health in people with severe mental illness. You can join in by following the #MindYourSmile hashtag on Twitter and tweeting your thoughts and comments with the hashtag in your tweets.
The poor physical health (including oral health) of people with severe mental illness (SMI) is a global challenge and policy priority in the United Kingdom (Firth et al. 2019). The Equally Well UK initiative and Closing The Gap Network are good places to start if you are new to this area.
The burden of oral diseases such as tooth decay, periodontal (gum) diseases, and tooth loss amongst people with SMI is substantial. This is due to their high prevalence and ability to precipitate and perpetuate SMI and other comorbid physical conditions. For example, systematic reviews have shown that people with SMI were nearly three times more likely to lose all their teeth and 50 times as likely to have periodontal disease compared to the general population (Kisely 2009; Kisely et al. 2015).
Oral diseases can cause poor nutrition and release pro-inflammatory cytokines that can induce chronic systemic inflammation (Hashioka et al. 2019; Sheiham et al. 2001). They can also cause chronic psychological stress due to associated pain and difficulties in sleeping, eating, speaking, smiling and experiencing discrimination and stigma related to poor dental appearance (Kusama et al. 2021; Moeller et al. 2015). All these implications of oral diseases are risk and prognostic factors for SMI and the comorbid physical conditions (Muller 2018; Stein et al. 2019). Thus, tackling oral diseases as part of the simultaneous treatment of the interlocked mental and physical conditions is of paramount importance.
Current guidance from NHS England and Improvement as well as the British Society for Disability and Oral Health (BSDOH) has stressed the importance of tackling oral diseases in people with SMI (Griffiths et al. 2000; Nursing Midwifery and Allied Health Professions Policy Unit 2016). However, a Cochrane review concluded that providing oral health education alone for people with SMI does not lead to a clinically meaningful improvement in oral health outcomes (Khokhar et al. 2016).
Since oral health education is only one type of a wider range of oral health interventions that could be offered to people with SMI, Macnamara et al. (2021) decided to carry out a systematic review to assess evidence on the effectiveness of oral health interventions of any type delivered to people with SMI.

People living with severe mental illness are nearly three times more likely to lose all their teeth and 50 times as likely to have periodontal disease compared to the general population.
Methods
The authors reported following the PRISMA guideline in reporting their systematic review and the registration of its protocol on PROSPERO database. They formulated a PICO question, where P (Population) was adult people with schizophrenia, bipolar disorders or other psychotic disorders, I (Intervention) was any intervention that was implemented with the aim of improving oral health, C (Comparator) was any comparator group and O (Outcome) was any clinical or proxy measure of oral health. Any interventional (analytical) study design was considered. No search period limit was applied, however, non-English studies were excluded.
The authors searched a wide range of appropriate databases including, inter alia, PubMed, Embase, CINAHL, PsychINFO and Cochrane library. They also searched abstracts of two international Psychiatry conferences and grey literature, and followed up from reference lists of included studies. Titles, abstracts and full texts were reviewed independently by two reviewers. Disagreements were discussed and resolved. Data extraction and risk of bias assessment were carried out independently by two reviewers using Cochrane risk-of-bias (RoB 2) tools for randomised controlled trials and cluster randomised controlled trials and the Risk of Bias in Non-Randomised Studies – of Interventions (ROBINS-I) tool for all other included study designs. The authors used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to score the quality of evidence. Due to clinical and methodological heterogeneity of included studies, meta-analysis was not performed and a funnel plot was not generated to assess publication bias.
Results
From a total of 1,465 unique citations, 12 studies met the eligibility criteria and were included in the review. To textually synthesise the findings, the authors grouped studies by outcome measure (clinical measures of oral health, measures of dry mouth, oral health knowledge and attitudes and oral health behaviours) and intervention type (dental education, motivational interviewing, dental checklist and incentivisation).
- Oral health education with or without motivational interviewing, incentives or provision of toothbrushes showed inconsistent findings across different clinical oral health measures.
- Several studies showed statistically significant improvements in measures of oral hygiene or plaque scores, however, such improvements were not clinically meaningful.
- Also, a statistically significant before-and-after effect was identified in relation to mouth dryness in one study (using subjective and objective measures of dry mouth).
- Furthermore, positive impacts on oral health knowledge, beliefs, attitudes and behaviours (such as brushing twice daily) were reported by several studies.
- With respect to dietary changes and dental treatment, one study tested the effect of providing two mangosteen fruits daily with non-surgical periodontal treatment compared to the latter alone. Although the study showed a statistically significant difference in gingival scores between the intervention and control group, no significant differences in plaque index, probing depth and clinical attachment level were reported.
- Interventions such as completing an oral health checklist by mental care coordinators about current oral health conditions and routines, coupled with an oral hygiene information sheet including information on how to find a dentist did not increase dental visits, owning a toothbrush or brushing twice daily.
The reviewers conclude that dental education shows promise as an intervention for people with severe mental illness, but further research is needed to provide more conclusive evidence.
Conclusions
The authors concluded that although some statistically significant improvement was seen in some clinical measures of oral health and toothbrushing behaviours there was no convincing evidence that oral health interventions identified led to clinically significant changes in oral health. Evidence on the effects of oral health education on plaque index was of moderate quality, whereas the quality of evidence for the remaining interventions was low or very low.
Strengths and limitations
The authors noted that searching a wide range of appropriate electronic databases supported by grey literature and a search of conference abstracts was a particular strength of their systematic review. However, excluding non-English studies due to lack of resources available for translation was a limitation. Selection bias was reduced by having two reviewers working independently of each other. Having broad eligibility criteria especially in relation to interventions and outcomes was noted by the authors as a potential limitation. The high clinical and methodological heterogeneity of included studies, which meant that some conclusions were based on the findings of one study, coupled with the high risk of bias in several studies was a further limitation.
There are other limitations beyond those noted by the authors. This systematic review considered a wide range of oral health interventions tested using various study designs. This could be considered a strength and limitation at the same time. For example, a randomised controlled trial (which is the gold standard in testing the effectiveness of interventions) might not be always ethical or feasible to conduct, as it is the case when evaluating policy or some community-based interventions. Thus, considering other types of study designs in such cases is appropriate. The authors should have provided rationale for including study designs other than randomised controlled trials. Furthermore, the grouping and labelling of interventions did not clearly follow a conceptual approach. For example, interventions that involved oral health education coupled with one or more of behaviour change techniques such as incentive and/or self-monitoring of behaviour could have been labelled as oral health behavioural interventions and data preferably would have been extracted in relation to the type and number of behavioural change techniques used. This could have given a richer picture to inform practice and future research. Finally, a realist approach to evidence synthesis (regarding what works for whom and in what context) could have also better informed future research and supported the development of complex intervention theory to tackle oral diseases amongst people with severe mental illness (SMI).

Following a conceptual approach in grouping interventions and extracting data could have given a more useful set of findings to inform practice and research.
Implications for practice
Similar to previous evidence syntheses in this topic, the authors stated that in the absence of definitive evidence for particular interventions, the BSDH oral health mental health guidelines should be followed. These guidelines promote a patient-centred approach to oral health promotion amongst people with severe mental illness (SMI) based on their individual health needs, such as type and severity of mental illness, living arrangements and physical health. They also recommended completing an oral health assessment and care plan, and educating healthcare professionals on addressing oral health needs through a multidisciplinary approach.
The authors of this systematic review encouraged clinicians, policy-makers and public health professionals to start asking questions about how oral health can be improved in people with SMI and called for future research to test interventions in different settings and patient groups and for longer follow-up periods. They also called for future research to explore how this may work in collaboration with existing strategies for physical health promotion.
The authors noted the little consideration of theory in included studies. They called for a participatory approach and conducting qualitative research to understand the acceptability of oral health interventions and how to address existing barriers to accessing dental care and maintaining good oral health amongst people with SMI.
There are other important implications beyond those noted by the authors. Due to the complex relationship between oral diseases and mental disorders and comorbid physical conditions and their intersectionality with the broader social determinants of health, it was not surprising to find that the provision of oral health education did not lead to clinically meaningful improvements in this group of people. Thus, there remains a need to develop, co-design and test complex interventions that are theory-driven and underpinned by systems thinking, coproduction and transdisciplinary approaches. This should start with setting research priorities (key uncertainties) and developing theory for complex interventions. Setting research priorities provides a systematic and transparent process to assist policy-makers and research funding agencies in making investment decisions to fund important research uncertainties that are relevant to the needs of people with mental disorders (Chalmers et al. 2014). An intervention theory is a pragmatic framework to describe how an intervention is expected to lead to its effects and under what conditions (Skivington et al. 2021).
These were the starting point for the two projects I am leading. One is a research priority setting about dental care in people with lived experience of severe mental distress called ‘RESTART dental care’ funded by Oral and Dental Research Trust. The other one is the MOOD study to explore multilevel barriers and facilitators to oral health and dental care utilisation amongst people with mental disorders funded by QMUL NIHR Clinical Lecturer Small Grant scheme. Anyone (service users with lived experience, carers, mental health and dental care professionals and commissioners) interested in taking part can find more details below.
RESTART Dental Care
Help us identify the Top 10 Research Priorities for Dental Care in People with Lived Experience of Severe Mental Distress. This online survey will take 5-mins to complete: https://qmul.onlinesurveys.ac.uk/restart-dental-care. The survey is aimed at people with lived experience of severe mental illness, family members and carers, and professionals or volunteers.

Take the RESTART survey now to improve dental care for people with severe mental illness.
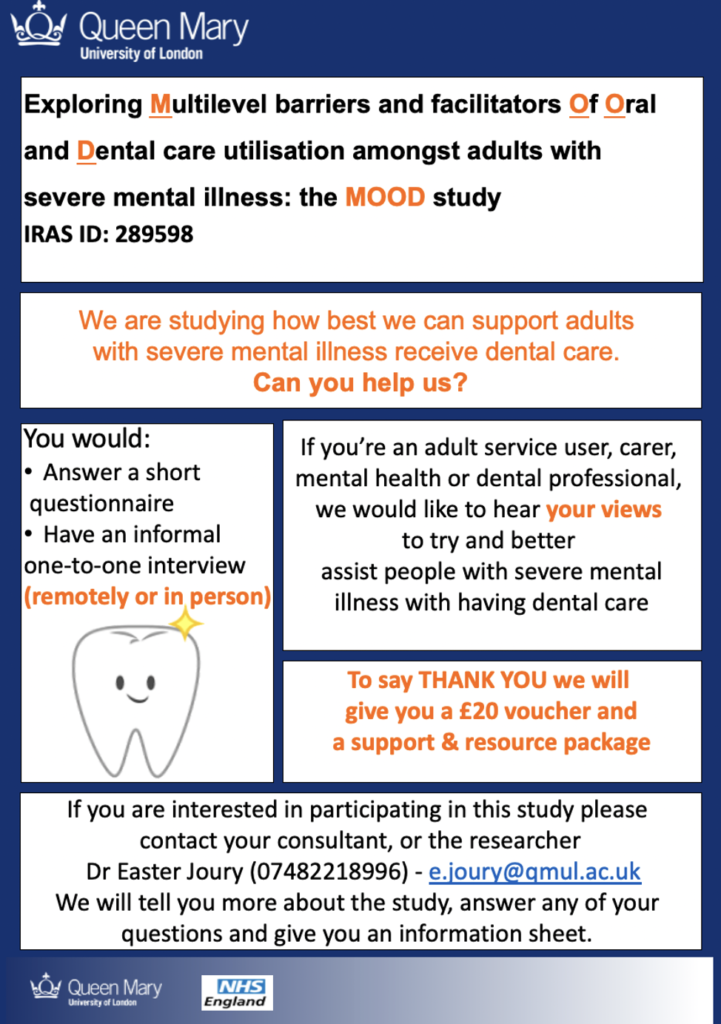
The MOOD Study
To participate in the MOOD study, please contact me (Easter Joury) on: e.joury@qmul.ac.uk or 07482218996.
If you want to find out more about the study you can download the patient information sheet (PDF), or the information sheet for carers, healthcare professionals and commissioners (PDF).
You can follow updates of both projects on:
Join the #MindYourSmile tweet chat
If you are interested in learning more, or sharing what you know about improving the oral health of people with severe mental illness, please join our #MindYourSmile tweet chat at 8-9pm on Monday 11th July. All you have to do to get involved is follow the #MindYourSmile hashtag and tweet your own thoughts and ideas about improving the oral health of people with severe mental illness.
Statement of interest
Easter Joury is leading two projects to support designing future complex interventions to improve oral health in people with SMI. This includes a research priority setting called RESTART dental care funded by Oral and Dental Research Trust and the MOOD study to explore multilevel barriers and facilitators to oral health and dental care utilisation amongst people with severe mental disorders funded by QMUL NIHR Clinical Lecturer Small Grant scheme.
Links
Primary paper
Macnamara A, Mishu MP, Faisal MR, Islam M, Peckham E. 2021. Improving oral health in people with severe mental illness (SMI): A systematic review. PLoS One. 16(12):e0260766.
Other references
Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, Howells DW, Ioannidis JP, Oliver S. 2014. How to increase value and reduce waste when research priorities are set. Lancet. 383(9912):156-165.
Firth J, Siddiqi N, Koyanagi A, Siskind D, Rosenbaum S, Galletly C, Allan S, Caneo C, Carney R, Carvalho AF, et al. 2019. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 6:675–712.
Griffiths J, Jones V, Leeman I, Lewis D, Blankenstein R. Oral Health Care for People with Mental Health Problems (PDF). BSDH Working Group; 2000.
Khokhar MA, Khokhar WA, Clifton AV, Tosh GE. 2016. Oral health education (advice and training) for people with serious mental illness. Cochrane Database Syst Rev. 9(9):CD008802.
Kisely S. 2009. A systematic review and meta-analysis of the oral health of psychiatric patients. Australian and New Zealand Journal of Psychiatry. 43(Suppl):A30-A31.
Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson NW. 2015. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med. 77(1):83-92.
Kusama T, Kiuchi S, Umehara N, Kondo K, Osaka K, Aida J. 2021. The deterioration of oral function and orofacial appearance mediated the relationship between tooth loss and depression among community-dwelling older adults: A JAGES cohort study using causal mediation analysis. J Affect Disord. 286:174-179.
Moeller J, Singhal S, Al-Dajani M, Gomaa N, Quiñonez C. 2015. Assessing the relationship between dental appearance and the potential for discrimination in Ontario, Canada.SSM Popul Health. 1:26-31.
Müller N. 2018. Inflammation in schizophrenia: pathogenetic aspects and therapeutic considerations. Schizophr Bull. 44(5):973-82.
Nursing Midwifery and Allied Health Professions Policy Unit. Improving the physical health of people with mental health problems: Actions for mental health nurses (PDF). Department of Health, Public Health England and NHS England; 2016.
Sheiham A, Steele JG, Marcenes W, Lowe C, Finch S, Bates CJ, Prentice A, Walls AW. 2001. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 80(2):408-413.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, Boyd KA, Craig N, French DP, McIntosh E, Petticrew M, Rycroft-Malone J, White M, Moore L. 2021. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 374:n2061.
Stein DJ, Benjet C, Gureje O, Lund C, Scott KM, Poznyak V, van Ommeren M. 2019. Integrating mental health with other non-communicable diseases. BMJ. 364:1295.
Photo credits
- Photo by Toa Heftiba on Unsplash