
There may be a couple less trees in the Woodland this year following a flurry of documents being published in relation to joining up physical and mental health care.
There was the Five Year Forward View for Mental Health from the NHS England Mental Health Taskforce Report which was published in February. There were 3 key findings from this, one of which was Bringing mental health care and physical health care together.
Soon after (March) the Kings Fund published the paper we will be focussing on today: Bringing together physical and mental health: a new frontier for integrated care which (in their own words) shows how this can be achieved.
Chris Naylor and team have produced a really useful, practical and pragmatic view of what can be done to improve the current situation; citing key services that are already doing this around the country; although at 122 pages it can be a little daunting! At the Kings Fund Conference on 8th March 2016, Chris Naylor did a fantastic 17 minute presentation summarising the paper, which can be found as an audio summary here. He did such a good job, that I have used some of his content here.
Integration and parity of esteem
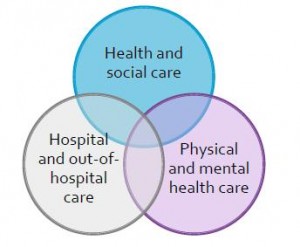
Integration is very much the buzz word within health care at the moment. In The Five Year Forward View (2014) Simon Stevens proposed the concept of triple integration, integrating:
- Health and social care,
- Hospital and out-of-hospital care, and
- Physical and mental health care.
This final area however appears to be slightly behind the other two and this needs to be addressed as soon as possible.
Parity of esteem is another well-worn phrase which on the surface implies mental health care being ‘as good as’ physical health care, however why not push further so that mental health is ‘part of’ care and not separate at all?
Why is this important?
The reasons why this is so important for patients are four fold:
- There are high levels of comorbidity between physical and mental health
- There is limited support for the wider psychological aspects of physical health and illness (especially long term conditions)
- There are persistent inequalities in life expectancy among people with severe mental illnesses (which is 15 – 20 years shorter)
- There is poor identification and management of medically unexplained symptoms.
In combination, this produces a human cost of poorer clinical outcomes and inequality of care and a financial cost to the NHS in excess of £11 billion per year.
Scope for improvement
The report identifies 10 areas where there is particular scope for improvement across the healthcare system;
Prevention/public health
- Incorporating mental health into public health programmes
- Health promotion among people with severe mental illnesses
General practice
- Improving management of ‘medically unexplained symptoms’
- Strengthening primary care for the physical health needs of people with severe mental illnesses
Chronic disease management
- Supporting the mental health of people with long term conditions
- Supporting the mental health and wellbeing of carers
Hospital care
- Supporting mental health in acute hospitals
- Addressing physical health in mental health inpatient facilities
Community care and social care
- Providing integrated support for perinatal mental heath
- Supporting the mental health needs of people in residential homes
There is unfortunately no ‘one size fits all’ solution to integration. But the core concepts should include:
- Redefining ‘core business’: broadening the scope of services to include the whole of the person
- Performing an educational function alongside a clinical one: skills can be transferred between clinicians just by working together
- Redesigning the workforce, e.g. through creation of new roles, for example liaison physicians (the mirror image of a liaison psychiatrist)
- Reducing stigma: the more we acknowledge mental health the easier it will be
But most importantly it is about getting the basics right. Staff having good communication skills and using language carefully. Thinking about the ‘whole person’ not just parts of the person and this isn’t about turning everyone into ‘experts in everything’, it is about joining together to synergistically enhance patient care.
Rethinking professional education
With the progression of specialisation (and sub-specialisation) within training, there will need to be a rethink within professional education across the range of knowledge, skills and behaviour so that all health and social care professionals have:
- Knowledge: awareness, knowledge of and identification of common conditions and risk factors
- Skills: a foundation of basic common competencies in mental and physical health care
- Behaviour: an openness to explore what a person’s wider needs might be beyond the boundaries of their own specialism, and an understanding of other forms of support that are available
This doesn’t necessarily mean re-inventing the wheel and may be a matter of:
Enhancing the skills and knowledge that are already present in most members of the…team but perhaps need reviving, refreshing and reinvigorating
– Elizabeth England, RCGP Clinical Champion for Mental Health and Whole Person Care 2014

The ownership challenge – it takes two to integrate.
Next steps
So, where do we go from here? Things that will help the process move faster include:
Leadership
- Developing passionate, skilful leaders
- Identifying board-level champions in provider organisations (both physical and mental health)
Financing and commissioning
- Involving commissioners at the outset
- Developing new payment systems and contracting mechanisms
Outcomes measurement
- Improving ability to demonstrate value
Harnessing digital technologies
- Integrating IT systems and using IT more innovatively

Leadership needs to come from all parts of the system.
Conclusions
Chris Naylor himself has said:
Traditionally physical and mental health have operated as distinct, separate systems in terms of both treatment and funding. That is no longer affordable financially or acceptable clinically.
There is a strongly compelling case for seeking to support mental and physical health in a more integrated way and there are lots of promising examples of local innovation outlined within the paper (which I would encourage you to take time to read). There does need to be consideration of how these can be scaled up though.
There are some broader implications for professional education and training which will require further thought and innovation in itself and finally we need the leadership from across the system to make this actually happen.
In essence what we are talking about is bringing two good things together, creating care which is greater than the sum of its parts. In musical terms this would be a mash up. Enjoy.
Links
Primary paper
Naylor C, Das P, Ross S, Honeyman M, Thompson J, Gilburt H. (2016) Bringing together physical and mental health. The King’s Fund, Mar 2016.
Other references
Farmer P, Dyer J. (2016) The Five Year Forward View for Mental Health. The Independent Mental Health Taskforce to the NHS in England, Feb 2016.
Stevens S. (2014) The Five Year Forward View. NHS England, Oct 2014.
England E. (2014) The extraordinary potential of primary care to improve mental health Royal College of General Practitioners. Clinical Resources. 2014

Today @LiaisonLawson publishes her 20th blog! It’s appropriately about integrating physical & mental health care https://t.co/p0P4Pzqrwf
Morning @chrisbnaylor @helengilburt Pls read @LiaisonLawson’s blog on your physical & mental health report https://t.co/p0P4Pzqrwf
Here’s the key points from the King’s Fund report on integrating physical & mental health services. https://t.co/kJYfMPzvLG
This looks fab @WeAHPs Pls read our blog today for some prep! https://t.co/p0P4Pzqrwf @LiaisonLawson https://t.co/UEZOXyRk1C
Thanks @LiaisonLawson for a great summary of why & how we need to integrate physical & mental health https://t.co/8uLGleeZfQ @Mental_Elf
Bringing together physical and mental health: King’s Fund report on integrated care https://t.co/AdPeMxR9yA via @sharethis
RT @Mental_Elf: There are high levels of comorbidity between physical and mental health https://t.co/p0P4Pzqrwf
RT @LiaisonLawson: Working with ITU about mental health. Integration of physical and mental health in action. More info at https://t.co/eig…
There’s limited support for wider psychological aspects of physical health & illness, esp. long term conditions https://t.co/p0P4Pzqrwf
Great summary and easy to read, sad that much of what you say needs doing to move forward has been said so many times before in different forms, Me thinks the time is right for action
There are persistent inequalities in life expectancy among ppl w severe mental illnesses (15–20 years shorter) https://t.co/p0P4Pzqrwf
Bringing together physical and mental health: King’s Fund report on integrated care https://t.co/enSeF6uhiy via @sharethis
RT @Mental_Elf: Don’t miss – Bringing together physical and mental health: King’s Fund report on integrated care https://t.co/p0P4Pzqrwf #E…
RT @AllenFrancesMD: Closely itegrating medical & mental health care greatly improves both & also reduces costs @Mental_Elf
https://t.co/54…
RT @Mental_Elf: Integrating physical & mental health requires leadership, financing/commissioning, outcome measurement & digital https://t.…
Thinking about the ‘whole person’ not just parts of the person – “@Mental_Elf: King’s Fund on integrated care https://t.co/6HVjvCbxJf #EBP”
King’s Fund report on integrated care proposes integrated perinatal mental health care https://t.co/MC5hREtSu1 via @EarlyPotential @AIMH16
Nice @Mental_Elf piece on integrating mental & physical health: for common MH IAPT expansion shd be integrated…
https://t.co/oTDWO8KDWg
RT @integrativpsych: Bringing together physical and #mentalhealth: @TheKingsFund report on integrated care https://t.co/6r94OPNBRq #physica…